Sample Clinical Notes: Templates & Expert Tips
In modern healthcare, the quality of your clinical notes directly impacts patient outcomes, legal standing, and operational efficiency. The pressure to document thoroughly while managing a demanding caseload often leads to burnout, with clinicians spending hours on administrative tasks. However, mastering the art of clear, concise, and accurate documentation is not just a best practice; it is a non-negotiable component of professional competence. Well-crafted notes ensure continuity of care, provide a robust legal record, and facilitate accurate billing and reimbursement.
This article moves beyond theory to provide practical, actionable tools. We will dissect six essential types of sample clinical notes, breaking down their structure, strategic purpose, and common pitfalls. Each example is designed to serve as a blueprint, helping you capture critical information efficiently without sacrificing detail. A critical aspect of mastering clinical notes involves adherence to regulations governing patient data. Professionals can find a comprehensive resource in the ultimate guide to handling Protected Health Information (PHI), which details the necessary safeguards.
You will gain access to strategic analysis and downloadable templates for the following essential documentation formats:
- SOAP Note (Subjective, Objective, Assessment, Plan)
- Psychiatric Mental Health Assessment Note
- Discharge Summary Note
- Progress Note
- Consultation Note
- Operative Note
By the end of this guide, you will have a clear framework for improving your documentation, saving valuable time, and enhancing the quality of care you provide. Let's dive into the examples.
1. SOAP Note (Subjective, Objective, Assessment, Plan)
The SOAP note is arguably the most recognizable and widely adopted format for clinical documentation in modern medicine. Developed by Dr. Lawrence Weed in the 1960s as part of the Problem-Oriented Medical Record (POMR), its structured framework is designed to promote clear, organized, and logical clinical reasoning. This method's enduring popularity, from bustling emergency departments to routine primary care follow-ups, stems from its simple yet powerful four-part structure.
Each letter in the acronym represents a distinct component of the patient encounter:
- S - Subjective: This section captures the patient's personal story. It includes the chief complaint, history of present illness, and any other information reported directly by the patient or their caregiver, such as symptoms, feelings, and personal history.
- O - Objective: This part contains concrete, observable, and measurable data. It includes vital signs, physical exam findings, laboratory results, and imaging reports. Crucially, this section should also document relevant negative findings (e.g., "no wheezing on auscultation").
- A - Assessment: Here, the clinician synthesizes the subjective and objective information into a clinical judgment. This includes the primary diagnosis, a list of differential diagnoses, and the status of any chronic conditions. Every assessment must be directly supported by the findings in the S and O sections.
- P - Plan: This final section outlines the strategy for patient care. It details the next steps, such as ordering further tests, prescribing medications, making referrals, and scheduling follow-up appointments. The plan should be specific, actionable, and include clear timelines.
Strategic Breakdown and Analysis
The SOAP note's primary strength is its logical flow, which guides the clinician from gathering information to forming a diagnosis and creating a treatment plan. This structured approach minimizes ambiguity and ensures that care decisions are well-documented and justified. For healthcare organizations, standardizing on the SOAP format improves communication between providers and creates a more consistent medical record for billing, compliance, and legal purposes.
The following infographic illustrates the fundamental workflow of creating a SOAP note, moving from patient-reported data to actionable treatment steps.
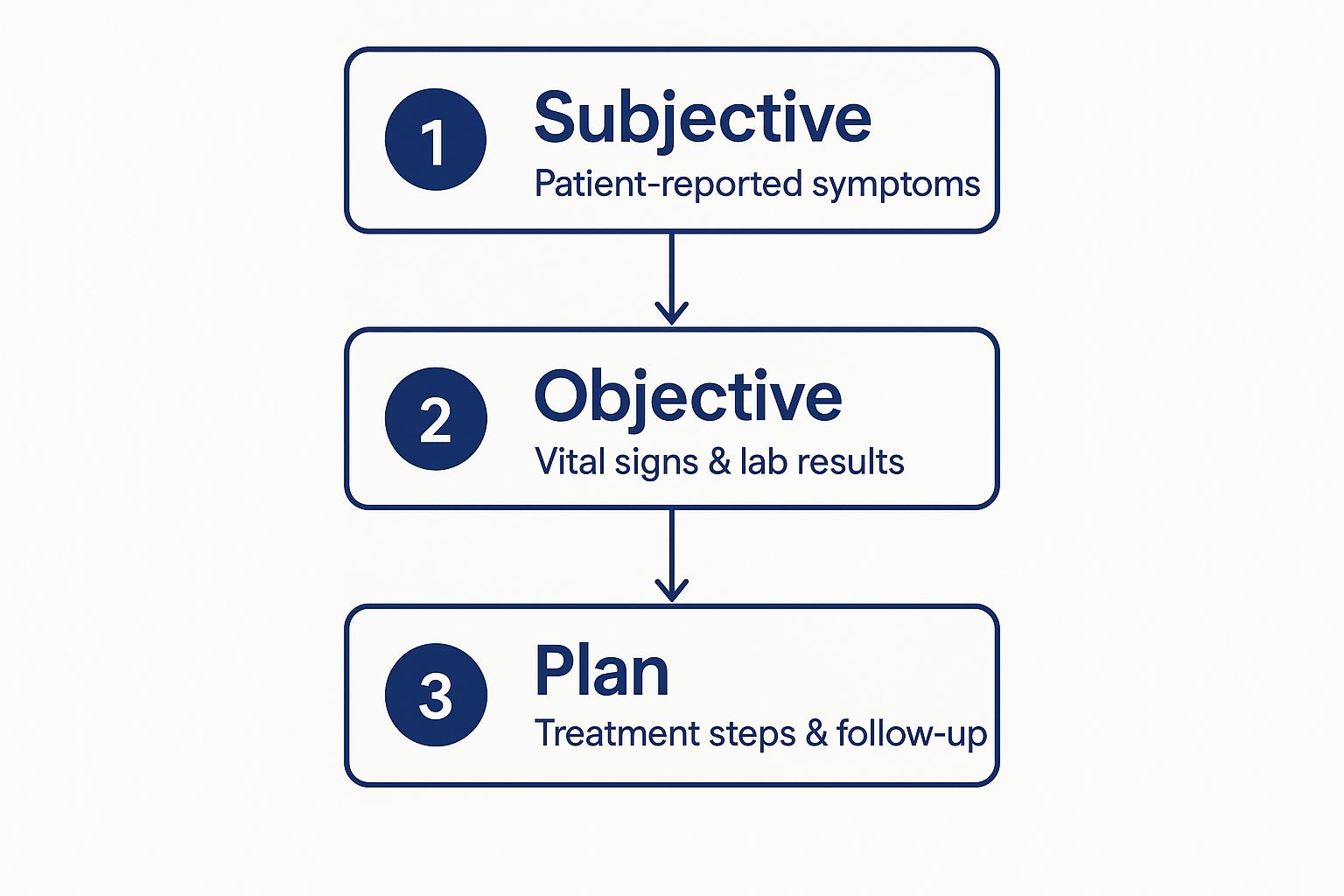
This visual process flow highlights how each stage builds upon the last, ensuring that the treatment plan is a direct and logical consequence of the documented subjective and objective findings.
Actionable Takeaways for Implementation
When implementing or refining the use of SOAP notes, focus on the connection between the sections. A common pitfall is a disconnect between the Assessment and the preceding information.
Key Tactic: Always cross-reference your Assessment against the Subjective and Objective sections. If you diagnose "acute bronchitis," the S section should mention a cough, and the O section should describe lung sounds like rhonchi or note the absence of pneumonia on a chest x-ray.
To enhance your documentation, consider these tips:
- Be Concise but Complete: Use precise medical terminology but avoid unnecessary jargon. Include pertinent negatives in the Objective section to show a thorough evaluation.
- Prioritize Problems: In the Assessment, list the most urgent or severe problem first. This helps focus the treatment plan and aids communication during handoffs.
- Make Plans Actionable: Instead of writing "follow up," write "follow up in 2 weeks to reassess blood pressure." This specificity improves patient adherence and continuity of care.
For healthcare providers looking to master this and other documentation techniques, you can find valuable strategies for improving clinical documentation on WhisperIT.ai. By mastering these clear and structured sample clinical notes, teams can ensure higher quality care and more robust record-keeping.
2. Psychiatric Mental Health Assessment Note
The Psychiatric Mental Health Assessment Note is a comprehensive documentation format tailored for evaluating a patient's mental state and psychiatric history. Unlike notes focused solely on physical health, this assessment delves into the complexities of thought, mood, behavior, and risk. Its structured approach is essential for accurate diagnosis, effective treatment planning, and ensuring patient safety in settings ranging from outpatient clinics to emergency departments.
This specialized note format integrates several critical components beyond a standard medical history:
- Identifying Information & Reason for Visit: Basic demographics and the patient's stated reason for seeking care, often including the source of referral.
- History of Present Illness (HPI): A detailed narrative of the current mental health symptoms, including onset, duration, severity, and impact on daily functioning.
- Past Psychiatric History: Previous diagnoses, hospitalizations, treatments (therapy and medications), and history of self-harm or suicide attempts.
- Mental Status Examination (MSE): A systematic observation of the patient's psychological functioning, covering appearance, behavior, speech, mood, affect, thought process, thought content, perception, cognition, insight, and judgment.
- Risk Assessment: An explicit evaluation of the patient's risk of harm to self (suicidal ideation) or others (homicidal ideation), including any specific plans, intent, or means.
Strategic Breakdown and Analysis
The primary strength of the psychiatric assessment note lies in its comprehensive and multi-faceted approach. It guides clinicians to gather both subjective reports and objective observations, creating a holistic picture of the patient’s mental health. This structure is mandated by regulatory bodies like The Joint Commission and aligned with best practices from the American Psychiatric Association to ensure a thorough, standardized evaluation.
This note format forces a clinician to move beyond a chief complaint and systematically explore all domains of mental functioning. Documenting a detailed MSE provides a crucial baseline, allowing future providers to track changes in a patient's condition over time. A well-documented risk assessment is not only vital for patient safety but also serves as critical legal and ethical protection for the provider and organization.
Actionable Takeaways for Implementation
When documenting a psychiatric assessment, the connection between the MSE, risk assessment, and the final treatment plan is paramount. A common mistake is documenting a plan that doesn't logically address the identified risks or symptoms.
Key Tactic: Directly link your safety plan to the findings in your risk assessment. If a patient reports suicidal ideation with a plan, the 'Plan' section must explicitly detail the interventions, such as creating a crisis response plan, removing access to means, or initiating hospitalization.
To enhance your documentation, consider these tips:
- Use Person-First Language: Write "a person with schizophrenia" instead of "a schizophrenic." This avoids stigmatizing labels and emphasizes the individual over the diagnosis.
- Document Key Quotes: For significant statements, especially regarding risk or psychosis, document the patient's exact words in quotation marks. This adds objective weight and clarity to your note.
- Integrate Collateral Information: When available, include information from family, friends, or previous providers. Note the source clearly (e.g., "Per patient's mother..."). This provides a more complete clinical picture.
- Make Safety Plans Concrete: Instead of "safety discussed," document the specific steps: "Patient contracted for safety, identified their sibling as a primary support, and was provided the national crisis line number: 988."
By mastering these detailed sample clinical notes, mental health professionals can ensure that their evaluations are thorough, compliant, and centered on patient safety and recovery.
3. Discharge Summary Note
The Discharge Summary is a critical clinical document that provides a comprehensive overview of a patient's entire hospital stay or treatment episode. Serving as the final chapter of an inpatient encounter, its primary purpose is to ensure a safe and effective transition of care from the hospital to the next setting, whether it be home, a rehabilitation facility, or another care provider. Mandated by regulatory bodies like the Joint Commission and the Centers for Medicare & Medicaid Services, this note is essential for maintaining continuity of care and preventing post-discharge complications.

A well-written discharge summary synthesizes a wealth of information into a concise, easily digestible format. Key components typically include:
- Admission and Discharge Diagnoses: The reason for hospitalization and the final diagnoses upon discharge.
- Hospital Course: A narrative summary of significant events, treatments, and the patient's response during their stay.
- Procedures and Consultations: A list of all surgical procedures, significant diagnostic tests, and specialist consultations.
- Discharge Condition: The patient's clinical status at the time of discharge (e.g., stable, improved).
- Discharge Medications: A detailed and reconciled list of all medications the patient should take after leaving the hospital, including dosage, frequency, and purpose.
- Follow-Up Instructions: Specific appointments, pending tests, and clear instructions for the patient and their next care provider.
Strategic Breakdown and Analysis
The strategic value of a high-quality discharge summary cannot be overstated. It acts as the primary communication tool between the hospital team and the outpatient providers who will assume care. A clear, accurate, and timely summary directly impacts patient safety, reduces the risk of readmission, and ensures therapeutic plans are continued without interruption. For the healthcare organization, robust discharge summaries are a cornerstone of quality improvement initiatives and regulatory compliance.
The document's structure is designed to answer key questions for the next provider: Why was the patient here? What happened to them? What is their current state? And what needs to happen next? This logical progression ensures that all critical information for post-discharge management is readily available, forming a vital part of the patient's permanent medical record. These and other sample clinical notes are key to effective care transitions.
Actionable Takeaways for Implementation
A common failure point in discharge summaries is ambiguity, particularly in medication reconciliation and follow-up plans. To avoid this, providers must focus on clarity and specificity.
Key Tactic: Implement a "closed-loop" communication process. This means not only providing written instructions but also verbally reviewing them with the patient or caregiver (using teach-back methods) and confirming that follow-up appointments are scheduled before the patient leaves the facility.
To improve your discharge documentation process, consider these tips:
- Ensure Timeliness: Complete the discharge summary within 24-48 hours of the patient's departure. Delays can lead to critical information gaps for the primary care physician.
- Focus on Medication Reconciliation: Explicitly state which medications were stopped, started, or changed. Explain the reason for any changes to prevent confusion and medication errors.
- Provide Actionable Follow-Up: Instead of "Follow up with PCP," write "Schedule appointment with Dr. Smith (PCP) at 555-123-4567 within 7-10 days to review lab results."
Properly managing these documents is crucial, and a modern healthcare document management system can streamline their creation, storage, and retrieval. Explore options for enhancing your facility's document workflow with a healthcare document management system from WhisperIT.ai. By standardizing these vital summaries, organizations can significantly improve patient outcomes and operational efficiency.
4. Progress Note
The Progress Note is the backbone of ongoing patient care documentation, serving as a dynamic record of a patient's journey through treatment. Unlike admission or discharge summaries that bookend a care episode, the progress note provides a serial, day-to-day account of a patient's condition. It is essential in settings like hospitals, rehabilitation centers, and long-term care facilities, where tracking incremental changes is vital for effective management.
This note format is designed to systematically document a patient's response to interventions and any changes from the previous assessment. Its core purpose is to ensure continuity of care, allowing any member of the healthcare team to quickly understand the patient's current status and the clinical reasoning behind any adjustments to the care plan.
The structure can vary, but it often includes:
- A brief summary: A one-line statement capturing the patient's current state and reason for ongoing care (e.g., "Post-op day 3, stable and ambulating").
- Subjective updates: Any new complaints, improvements in symptoms, or concerns reported by the patient or their family since the last note.
- Objective data: Updated vital signs, new lab or imaging results, and relevant physical exam findings, with a focus on changes.
- Assessment: A re-evaluation of the active problems, noting whether they are improving, worsening, or resolved.
- Plan: Adjustments to the treatment plan for each active problem, including changes in medication, new orders, or consultations.
Strategic Breakdown and Analysis
The primary strength of the progress note lies in its focus on change and continuity. By design, it compels clinicians to compare the patient's current state to their previous one, preventing stagnant care plans and promoting proactive adjustments. This systematic tracking is crucial for meeting regulatory and billing requirements, such as those from Medicare, which mandate clear evidence of ongoing medical necessity.
In a multi-provider environment, these notes are the primary communication tool. A well-written progress note ensures that a covering physician or a consulting specialist can seamlessly take over care, fully informed of the patient's trajectory and the rationale for the current treatment strategy. This systematic approach reduces the risk of medical errors and enhances team collaboration.
Actionable Takeaways for Implementation
When writing progress notes, efficiency and clarity are paramount. The goal is to convey the most critical information without redundant detail from previous entries.
Key Tactic: Adopt a "by-problem" or "by-system" approach. Instead of a narrative that mixes issues, organize your Assessment and Plan by a numbered problem list (e.g., 1. Pneumonia, 2. Acute Kidney Injury, 3. Hypertension). Address the status and plan for each one individually, which streamlines clinical reasoning.
To elevate your progress note documentation, consider these tips:
- Focus on the "So What?": Don't just list data. Explain its significance. Instead of "K 3.1," write "Hypokalemia, will replete with K-Dur 40mEq PO x1."
- Document Communication: Note any significant conversations with the patient, family, or consultants. This is crucial for care coordination and legal documentation.
- Be Specific About Progress: Quantify changes whenever possible. "Wound decreased in size from 2 cm to 1.5 cm" is more valuable than "wound improving."
For busy clinicians, tools like medical dictation software can significantly speed up the creation of these detailed sample clinical notes. You can find valuable strategies for integrating this technology on WhisperIT.ai. By mastering these structured progress notes, teams can maintain high standards of care while improving documentation efficiency.
5. Consultation Note
A Consultation Note is a specialized report authored by a consulting specialist following a referral from another healthcare provider. Its purpose is to provide an expert opinion, targeted assessment, and specific recommendations regarding a particular medical problem or clinical question. This document is a cornerstone of collaborative care, bridging the gap between general practice and specialized medicine, such as a cardiologist evaluating chest pain or a surgeon assessing a patient for a potential operation.
The format is structured to communicate findings clearly and directly back to the referring provider. Key components include:
- Reason for Consultation: A clear statement of the specific question being asked by the referring provider (e.g., "Evaluation of new-onset atrial fibrillation").
- History and Findings: A focused summary of the patient's history, physical examination, and diagnostic results that are pertinent to the consultation question.
- Impression/Assessment: The consultant’s expert clinical judgment and diagnosis, directly addressing the reason for the referral.
- Recommendations: A clear, actionable set of recommendations for treatment, further testing, or management. This is the most critical part of the note.
Strategic Breakdown and Analysis
The primary strength of a well-written Consultation Note lies in its clarity and directness. Unlike a comprehensive history and physical, its scope is intentionally narrow, focusing only on the specific question at hand. This precision ensures that the referring provider receives unambiguous, actionable guidance, which enhances patient safety and care efficiency. The note serves as a formal record of the specialist’s involvement and recommendations, crucial for continuity of care and medicolegal documentation.
For healthcare organizations, standardizing the format for these sample clinical notes improves inter-departmental communication and reduces the risk of misinterpreted advice. A successful consultation hinges on the prompt and clear transmission of this vital information between providers.
Actionable Takeaways for Implementation
The most common failure in consultation documentation is providing vague or non-committal recommendations. To be effective, the note must guide the referring clinician’s next steps.
Key Tactic: Structure your "Recommendations" section as a numbered list with explicit actions. Directly answer the consultation question in your first recommendation, and clearly state the urgency of each subsequent step (e.g., "Urgent," "Within 2 weeks").
To elevate the quality of your consultation notes, consider these tips:
- Address the Question Directly: Begin your assessment by restating and directly answering the referral question. This immediately provides the key information the referring provider needs.
- Be Decisive: Offer clear, evidence-based recommendations. Instead of "consider cardiology follow-up," write "Recommend follow-up with our clinic in 4 weeks to monitor response to metoprolol."
- Close the Loop: Ensure the note is sent promptly to the referring provider. Effective communication is as important as the clinical opinion itself. This process often involves sharing documents between different EMR systems.
For teams navigating the complexities of sharing specialist reports and other protected health information, understanding secure methods is paramount. You can explore best practices for HIPAA-compliant document sharing on WhisperIT.ai. By mastering these targeted communication skills, specialists can significantly improve collaborative care outcomes.
6. Operative Note
The Operative Note is a critical legal and medical document that provides a detailed, moment-by-moment account of a surgical procedure. Its primary function is to serve as a comprehensive, permanent record of the entire surgical event, from the preoperative diagnosis to the final instrument count. Mandated by regulatory bodies like the Joint Commission and championed by organizations such as the American College of Surgeons, this note is essential for ensuring continuity of care, facilitating communication between providers, and protecting both the patient and the surgical team from a medicolegal standpoint.
Unlike other sample clinical notes, the Operative Note follows a highly standardized format that leaves little room for ambiguity. Its key components typically include:
- Preoperative and Postoperative Diagnosis: The initial diagnosis justifying the surgery and the final diagnosis confirmed by the procedure.
- Procedure Performed: The official name of the surgery using standardized terminology (e.g., "Laparoscopic Cholecystectomy").
- Surgeon and Assistants: A complete list of all medical personnel involved in the operation, including their specific roles.
- Anesthesia: The type of anesthesia administered and the name of the anesthesiologist.
- Findings: A detailed description of the anatomical structures and any pathology observed during the surgery.
- Procedure Description: A step-by-step narrative of the surgical technique, including incisions, dissections, resections, and repairs.
- Specimens: Any tissue or fluid removed for pathological analysis.
- Complications: A transparent account of any adverse events or deviations from the planned procedure.
- Closure and Counts: Details on how the incision was closed and confirmation that all sponges, needles, and instruments were accounted for.
Strategic Breakdown and Analysis
The strength of the Operative Note lies in its meticulous and chronological structure, which creates an unassailable record of care. This documentation is not just a medical report; it is a legal safeguard that substantiates the quality and appropriateness of the care delivered. For healthcare systems, enforcing timely and complete operative note documentation is a cornerstone of risk management and quality assurance programs. The detailed narrative provides invaluable data for peer review, quality improvement initiatives, and research.
The video below offers a practical guide on structuring and dictating an effective operative report, emphasizing clarity and completeness.
This structured approach ensures every critical element of the surgery is captured, supporting postoperative care handoffs and long-term patient management.
Actionable Takeaways for Implementation
The most significant challenge with operative notes is timeliness and accuracy. Details fade quickly, making immediate post-procedure documentation essential.
Key Tactic: Dictate or write the operative note immediately following the procedure. Do not leave the operating suite until the core details are captured. This practice drastically reduces the risk of errors and omissions.
To improve the quality of your operative notes, consider these tactical tips:
- Use a Template: Standardize your operative notes using a pre-defined template for each common procedure. This ensures all required fields are completed and improves efficiency.
- Be Specific and Objective: Avoid vague terms. Instead of "difficult dissection," describe why it was difficult (e.g., "extensive adhesions between the gallbladder and liver requiring sharp dissection").
- Document Deviations: Clearly state any variation from the standard or planned procedure and provide a clinical justification for the change. This is crucial for both patient safety and legal protection.
By optimizing the creation of these notes, surgical departments can enhance patient outcomes and operational efficiency. You can discover more about integrating these documentation practices with broader institutional improvements by learning about workflow automation in healthcare at WhisperIT.ai. Mastering this format is non-negotiable for any practicing surgeon.
Comparison of 6 Sample Clinical Notes
| Documentation Type | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| SOAP Note | Moderate; standardized four-section format | Moderate; requires time for thorough data entry | Systematic patient assessment, supports clinical decision-making | ED complaints, primary care, specialist consults | Promotes communication, legal compliance, quality improvement |
| Psychiatric Mental Health Note | High; specialized mental health knowledge needed | High; specialized training and assessment tools | Comprehensive mental health evaluation and risk assessment | Psychiatric evaluations, mental health emergency | Standardized risk protocols, supports safety planning |
| Discharge Summary Note | Moderate to High; detailed summary needed | Moderate; coordination with multiple departments | Continuity of care, regulatory compliance | Hospital stays, surgical discharges, rehab | Ensures care transition, regulatory and billing compliance |
| Progress Note | Low to Moderate; brief daily updates | Low; frequent documentation required | Tracks patient progress, aids daily decision-making | Daily inpatient notes, outpatient treatments | Facilitates communication, quick completion |
| Consultation Note | Moderate; requires specialist input | Moderate; coordination between providers | Expert opinion and recommendations for complex cases | Specialist referrals, complex case evaluation | Provides expertise, improves care quality and coordination |
| Operative Note | High; detailed surgical documentation required | High; surgical team input needed | Complete surgical record, legal documentation, postoperative care | Surgical procedures across specialties | Critical legal document, quality improvement, billing |
Streamline Your Documentation: The Future of Clinical Note-Taking
Throughout this guide, we've dissected a diverse collection of sample clinical notes, from the structured SOAP note to the comprehensive discharge summary. We've explored the specific requirements of psychiatric assessments, the focused narrative of progress notes, the collaborative nature of consultation notes, and the meticulous detail of operative reports. While each document serves a unique purpose within the patient's journey, a set of universal principles underpins them all.
Effective clinical documentation is a delicate balance. It must be detailed enough for legal and medical continuity, yet concise enough to be efficient. It demands unwavering accuracy to ensure patient safety and clear communication to facilitate collaborative care. Mastering this skill is not just about filling out forms; it's about creating a powerful, reliable record that protects patients, informs colleagues, and validates the high-quality care being delivered.
Synthesizing Core Strategies for Effective Documentation
Across all the sample clinical notes we analyzed, several core strategies consistently emerged as best practices. Moving beyond the specific templates, these are the high-level takeaways that can transform your documentation process from a necessary chore into a strategic asset.
- Structure is Your Foundation: Whether you use the SOAP, DAP, or another framework, a consistent structure is non-negotiable. It creates a predictable flow of information, making it easier for you to write and for others to read and quickly find the information they need.
- Objectivity is Paramount: Stick to observable facts and quantifiable data wherever possible. Use direct quotes for subjective patient statements, but avoid interpretive or judgmental language. This practice is crucial for medical accuracy and legal defensibility.
- Clarity Through Conciseness: Eliminate jargon, vague terms, and redundant phrases. The goal is unambiguous communication. As seen in our progress and consultation note examples, a well-written note gets straight to the point, saving time for every professional who reads it.
- The "Why" Behind the "What": Your assessment and plan are the heart of the clinical note. Don't just list diagnoses and treatments; connect them. Clearly articulate your clinical reasoning, explaining why a particular diagnosis is being considered and how the proposed plan will address the patient's specific problems.
Key Insight: The true value of a clinical note isn't just in the information it contains, but in the clinical reasoning it demonstrates. It tells a story of thoughtful, evidence-based care.
Bridging the Gap with Modern Technology
The principles of great documentation are timeless, but the tools we use to achieve them are evolving rapidly. The administrative burden of manual note-taking is a well-documented source of professional burnout, directly impacting the time available for patient interaction. This is where technology offers a transformative solution, moving us from simply understanding what a good note looks like to implementing a workflow that produces them efficiently.
Modern tools are designed to automate the most tedious parts of documentation. For those looking to enhance efficiency, exploring the role of AI in text creation can significantly streamline the clinical documentation process. Advanced AI-powered dictation services can now transcribe conversations with near-perfect accuracy, while intelligent templating systems can auto-populate routine information, freeing you to focus on the nuanced details of the assessment and plan.
By embracing these innovations, you are not cutting corners; you are optimizing your workflow. You are leveraging technology to handle the repetitive tasks, allowing your clinical expertise to shine through in the most critical sections of your notes. This strategic adoption empowers you to create comprehensive, accurate, and compliant documentation in a fraction of the time, directly translating to more time for what matters most: your patients.
Ready to revolutionize your clinical documentation workflow? Discover how Whisperit uses advanced AI to turn your spoken words into perfectly structured, accurate clinical notes. Reclaim your time and eliminate documentation headaches by exploring our secure, intuitive platform today. Visit Whisperit to learn more.