Top Medical Voice Recognition Software for Healthcare
Navigating the Medical Voice Recognition Software Revolution
Healthcare documentation is undergoing a major change, moving well beyond basic dictation tools. The era of slow, error-filled transcription is giving way to a new class of intelligent software. This shift is not just about convenience; it is a direct solution to a significant problem in modern medicine: the administrative overload on clinicians. Old documentation methods, which involve heavy manual data entry, are a known cause of physician burnout, affecting both patient care and job satisfaction.
From Transcription to Intelligent Automation
The primary issue with older systems is their lack of clinical context. They process medical notes as plain text, unable to grasp the structure, relationships, and data points essential for effective electronic health records (EHRs). In contrast, modern medical voice recognition software functions as a clinical assistant driven by artificial intelligence. These advanced platforms are built to:
- Comprehend complex medical terms across different specialties.
- Isolate and ignore background noise typical in clinical environments.
- Identify and learn various accents and speech patterns.
- Automatically structure dictated notes into standard formats like SOAP notes.
This means a doctor can converse naturally with a patient while an ambient listening tool captures the dialogue, isolates clinically relevant details, and populates the EHR automatically. Moving from active dictation to this passive, intelligent capture method marks a substantial improvement in workflow.
Real-World Transition and Growth
Healthcare organizations that adopt modern medical voice recognition software often see major improvements. For instance, top platforms now offer smooth integration with major EHRs, eliminating the workflow disruptions that hindered earlier adoption. The screenshot below illustrates how a current platform positions its documentation solutions as a core part of the clinical workflow, not an add-on tool.

The image underscores a key point: the goal is to reduce the cognitive load on physicians by automating clinical documentation within their existing processes, leading to better efficiency and accuracy. While the initial setup and learning period can pose some difficulties, the long-term gains—like less time spent on documentation and higher-quality notes—are powerful reasons for this technological shift.
Market data supports this trend. The global medical speech recognition software market was valued at about USD 1.73 billion in 2024 and is expected to grow to USD 5.58 billion by 2035. This growth is driven by the increasing need for clinical efficiency, progress in AI, and the rise of telehealth. You can find more details on these market trends in the full medical speech recognition software market report. This expansion highlights the industry's focus on finding lasting solutions to documentation problems.
Understanding What Makes Medical Voice Recognition Actually Work
A flashy demonstration is one thing, but consistent performance in a busy clinical setting is entirely different. The true worth of medical voice recognition software is found in its core architecture and its ability to manage real-world clinical chaos. What separates a helpful tool from a frustrating one is how it processes speech, integrates with existing systems, and adapts to the unpredictable nature of healthcare.

The image of the Epic Systems website hints at the complex digital ecosystem where these voice tools must function. Smooth integration is not a luxury but a basic requirement for user adoption and success. This is why the choice between deployment models—cloud-based versus on-premises—is so important. A cloud solution provides great scalability and access to the latest AI models, while an on-premises system gives an organization full control over its data, a vital consideration for certain security protocols.
Accuracy in the Real World
Published accuracy rates, often stated as exceeding 99%, are typically measured under ideal, quiet conditions. However, a real clinic is filled with background conversations, medical equipment alarms, and other ambient sounds. The best software uses advanced noise cancellation and speaker diarization (distinguishing who is speaking) to maintain high accuracy despite these disturbances. To truly appreciate the capabilities of these tools, it helps to understand the core principles behind effective interactive voice recognition (IVR) systems, which face similar challenges in isolating user speech from environmental noise.
The importance of this technology is expanding quickly. Valued at approximately USD 2.1 billion in 2024, the global market for voice technology in healthcare is projected to reach USD 12.5 billion by 2037. This expansion is directly linked to the documentation demands for the more than 1.5 billion people worldwide with chronic diseases. You can explore more about the trends in the healthcare voice technology market and its expected growth.
Front-End vs. Back-End Recognition
The operational model of medical voice recognition software also significantly affects a physician's workflow. The two main models are front-end and back-end recognition, each with distinct effects on daily use.
- Front-End Recognition: This is real-time transcription. As a clinician speaks, the text appears on their screen instantly. This allows for immediate review and editing, making it suitable for physicians who prefer to sign off on notes at the point of care. The direct feedback loop helps the AI learn the user's speech patterns more quickly.
- Back-End Recognition: In this model, the clinician dictates into a recorder, and the audio file is sent to a server for processing. The transcribed text is returned later for review, often by a medical transcriptionist who edits it for accuracy before the physician signs off. This approach is less disruptive during patient encounters but delays the final documentation.
The choice between these models depends entirely on a clinic’s workflow needs. A fast-paced emergency department might favor back-end systems to keep physicians moving, while a primary care practice may prefer the immediate finality of front-end recognition to close charts the same day. Ultimately, the most effective medical voice recognition software is the one that aligns with and improves existing clinical processes rather than forcing users into a new, inefficient routine.
Platform Deep Dive: What Really Sets Leading Solutions Apart
Beyond accuracy claims, the true value of a medical voice recognition software platform is proven in daily clinical practice. The differences between market leaders are often nuanced but carry significant weight for workflow efficiency, total cost, and physician adoption. Analyzing the distinct philosophies of major players—from established incumbents to cloud giants and AI-native startups—helps clarify which solution best fits specific clinical environments.
The Incumbent vs. The Cloud Giants
On one end of the spectrum sits Dragon Medical One by Nuance, a specialized, deeply embedded solution refined over decades. Its core strength is its vast, pre-built medical vocabularies, which cover more than 90 medical specialties. For a cardiologist or oncologist, this means the software understands their specific terminology from day one, substantially reducing the initial training period. Dragon's design is clinician-centric, aiming to perfect the front-end, real-time dictation experience directly within the EHR. This makes it a formidable choice for practices that demand high out-of-the-box accuracy for complex medical language.
In contrast, platforms like Amazon Transcribe Medical and Google Cloud's Healthcare API offer a different architectural model based on massive, scalable cloud infrastructure. Their primary advantage lies not in specialty-specific lexicons but in providing powerful, flexible, and cost-effective raw transcription. For a large hospital system building a custom telehealth application or a clinic developing its own ambient documentation tools, these platforms offer essential building blocks. They are excellent at processing high volumes of audio and provide APIs for deep, custom integrations, though they typically require more development work to fine-tune for specific clinical workflows.
The Rise of AI-Native Assistants
A newer category has emerged with platforms such as Suki AI. These solutions move beyond simple transcription to function as AI-powered clinical assistants. Suki focuses on reducing the number of commands a physician must learn by using natural language understanding to interpret intent. A doctor might say, "Suki, order a complete blood count," and the system understands the command, locates the correct order in the EHR, and queues it. This approach directly confronts physician burnout by tackling "click fatigue"—the exhaustion from navigating intricate EHR interfaces.
To provide a clear, side-by-side view, the following table breaks down how these leading platforms perform against critical decision-making criteria.
Leading Medical Voice Recognition Platforms Comparison
Real-world performance analysis of accuracy rates, specialty support, integration capabilities, and deployment options across major platforms
| Platform | Clinical Accuracy | Specialty Focus | EMR Integration | Deployment Model | AI Capabilities |
|---|---|---|---|---|---|
| Dragon Medical One | High out-of-the-box accuracy for complex terms; requires minimal training. | Extensive; over 90 pre-built vocabularies for medical specialties. | Deep, seamless integration with all major EHRs for front-end dictation. | Cloud-based SaaS (Software as a Service) | Real-time speech-to-text, voice navigation, ambient intelligence (DAX). |
| Amazon Transcribe Medical | High general medical accuracy; may require tuning for niche specialties. | General medicine; designed to be customized via machine learning. | API-based; requires development work for custom integration. | Cloud-based PaaS (Platform as a Service) | Batch and real-time transcription, speaker identification, custom vocabulary. |
| Google Healthcare API | Strong accuracy backed by Google's ML; requires developer configuration. | Broad medical focus; adaptable for various clinical contexts. | API-based; designed for developers building custom health apps. | Cloud-based PaaS | Natural Language API for extracting medical insights, data de-identification. |
| Suki AI | High accuracy focused on conversational commands and documentation. | Primarily focused on high-volume specialties like primary care and cardiology. | Integrates with leading EHRs to automate tasks beyond dictation. | Cloud-based SaaS with a focus on mobile and web app. | AI assistant for voice-enabled orders, diagnosis coding, and queries. |
This comparison shows a clear divergence in strategy. Dragon offers a polished, turnkey solution for dictation, while Amazon and Google provide the raw power for custom projects. Suki, on the other hand, aims to reduce administrative burden through a more interactive AI model.
The industry is also moving toward ambient clinical intelligence, which passively captures and documents patient encounters without active dictation.

This image highlights the shift from active commands to a passive, AI-driven process that understands conversational context—a key feature of next-generation tools. This evolution toward ambient documentation is a central theme in the development of medical speech to text software, aiming to make technology disappear into the background of the patient-physician interaction.
Ultimately, the right platform is determined by the problem it needs to solve. For unmatched, specialty-specific dictation accuracy, Dragon remains a top contender. For scalable, adaptable transcription to power custom applications, Amazon and Google provide the foundational technology. For a solution built to reduce administrative work through AI assistance, Suki presents a compelling alternative.
Security and Compliance: What Actually Matters in Practice
When choosing a medical voice recognition software, viewing HIPAA compliance as the starting point, not the ultimate goal, is essential. While nearly every vendor asserts compliance, the real-world application of their security measures varies significantly, which directly affects patient data protection and your organization's liability. The critical question isn't just about having a Business Associate Agreement (BAA), but how the software's architecture actively secures Protected Health Information (PHI) during daily clinical use.
The move to digital health records amplifies these concerns. In the United States, the hospital adoption rate for electronic health records (EHRs) has reached nearly 97.4%. This high adoption rate increases the need for secure voice tools that can integrate with these systems. Consequently, global R&D investments in healthcare voice recognition went past USD 2.5 billion in 2024, driven by the demand for secure, often cloud-based, solutions. You can learn more by reviewing the latest research on the voice technology in healthcare market.
Data Encryption: In-Transit vs. At-Rest
A key difference among platforms is how they handle data encryption. It's not sufficient for data to be encrypted; you need to understand when and where that encryption occurs. A robust security framework addresses two distinct states:
- Encryption in-transit: This protects data as it moves from a clinician's microphone to the vendor's server for processing. Look for solutions that use strong protocols like TLS 1.2 or higher to prevent interception during transmission.
- Encryption at-rest: This secures data once it is stored on a server, whether as a temporary audio file or a finalized text document. Industry standards like AES-256 encryption are crucial for this stage.
A vendor that excels in one area but is unclear about the other creates a potential vulnerability. For example, an audio file sent unencrypted over a hospital’s Wi-Fi network before being securely stored in the cloud represents a major security gap. Your evaluation must confirm end-to-end encryption. For more details on this topic, our guide on HIPAA compliant transcription offers a complete breakdown of the requirements.
Access Controls and Data Storage Models
Beyond encryption, practical security depends on who can access data and where it is stored. The U.S. Department of Health and Human Services outlines the necessary administrative, physical, and technical safeguards under HIPAA.
This guidance underscores that compliance is a broad effort, extending beyond just technology to include internal policies and procedures. Your choice of data storage model directly influences these safeguards. A cloud-based system centralizes data on the vendor's servers, which can provide sophisticated security monitoring but requires trusting a third party's infrastructure. In contrast, an on-premises solution keeps all PHI under your organization's direct control, simplifying data residency issues but placing the entire responsibility of securing servers and networks on your IT department.
Ultimately, a vendor's security claims need to be supported by a transparent architecture and auditable controls. Your due diligence should involve a detailed security questionnaire probing these specific areas. It's also important to understand the broader context of data protection; exploring best practices for improving patient data security in healthcare IT can help you build a more resilient security posture. Choosing a partner with a demonstrable, layered security strategy is vital for protecting both your patients and your practice.
Real Implementation Stories: Learning from Success and Failure
The theoretical advantages of medical voice recognition software—like less time spent on documentation, reduced burnout, and better notes—are only meaningful if they hold up in a busy clinical environment. By looking at real-world rollouts, we can identify the critical factors that distinguish a successful deployment from a frustrating one. These stories offer a practical guide for anticipating challenges and getting the most from this technological investment.
Success Story: The 400-Bed Hospital System
A 400-bed hospital system provides a clear example of a successful deployment. Their main objective was to cut down on documentation time, a major source of physician dissatisfaction. The implementation resulted in a 40% reduction in the average time spent on documentation per patient encounter.
This outcome was not accidental. It was the result of several deliberate strategic decisions:
- Clinical Champions: The hospital identified respected physicians in each department to serve as advocates. These champions got advanced training and helped customize templates and macros for their specialties, making the system immediately useful to their colleagues.
- Phased Rollout: Instead of a single "go-live" event across the entire system, they introduced the software one department at a time. They began with specialties like radiology and pathology, where dictation was already a common practice. This strategy allowed the IT team to address problems on a smaller scale and use what they learned for future rollouts.
- Mandatory, Personalized Training: Every physician was required to attend a one-on-one training session. This made sure everyone was comfortable with the essential functions and voice commands, which helped prevent initial frustration that could lead to abandoning the tool.
Failure Story: The Multi-Specialty Clinic
In a contrasting case, a multi-specialty outpatient clinic saw its implementation stall, even though it had invested in a similar high-quality platform. Six months after the launch, user adoption was under 20%. Most physicians had gone back to typing their notes manually or using traditional transcription services.
An analysis after the fact revealed several critical errors:
- Lack of Workflow Analysis: The clinic's IT department selected the software based on its features and price tag, without a thorough analysis of the specific workflows in each specialty. The chosen front-end system disrupted the workflow for urgent care physicians, who needed a faster, back-end dictation model to keep pace.
- Generic, One-Size-Fits-All Training: The clinic offered optional group training sessions that didn't cater to the documentation needs of different specialties. For instance, a dermatologist's need to describe skin lesions is fundamentally different from a cardiologist's need to detail heart sounds.
- Ignoring User Feedback: Early complaints about the software's initial accuracy and integration problems were brushed off as simple "resistance to change." This approach alienated the clinical staff and fostered the view that the new system was being imposed on them without adequate support, which stopped any chance of organic adoption.
Lessons Learned for Successful Implementation
These stories show that technology is just one piece of the puzzle; human factors are just as important. Leading institutions such as the Mayo Clinic focus on integrating technology in a way that supports, rather than disrupts, a physician's work.
This image reflects a philosophy where technology serves the primary mission of patient care, a core principle for any software implementation. The main lesson is that successful adoption hinges on aligning the tool with existing clinical processes and culture. You can discover more about applying these concepts by exploring strategies for healthcare process improvement that put workflow at the heart of technological change.
The most crucial takeaway is that a medical voice recognition software project is a change management initiative first and a technology project second. By concentrating on clinical workflows, getting buy-in through champions, and offering tailored support, healthcare organizations can steer clear of common issues and realize the full benefits of voice-driven documentation.
Making the Financial Case: Beyond Initial Costs
Calculating the return on investment for medical voice recognition software requires looking far beyond the initial subscription or licensing fees. A successful financial justification accounts for the total cost of ownership (TCO) and measures benefits that extend beyond simple time savings. The true value emerges when you analyze the complete financial picture, including both direct expenses and indirect gains that impact your organization's bottom line and clinical quality.
Deconstructing the Total Cost of Ownership
To build a realistic budget, healthcare leaders must consider several cost categories that are often overlooked in initial proposals. These "hidden" expenses are critical for a smooth implementation and sustained adoption.
- Initial Implementation & Integration: This includes one-time fees for integrating the software with your existing Electronic Health Record (EHR) system. Depending on the vendor and your IT infrastructure, this can be a significant cost.
- Training & Onboarding: Effective training is essential. Budget for personalized training sessions for clinical staff, recognizing that a one-size-fits-all approach often fails. Factor in the cost of reduced physician productivity during this initial learning phase.
- Ongoing Support & Maintenance: Most vendors offer tiered support plans. A basic plan might be included, but premium, 24/7 support for a mission-critical system will come at an additional annual cost.
- Infrastructure Upgrades: Cloud-based solutions minimize this, but on-premises software may require server upgrades or enhanced network security measures.
To help visualize these financial components, the following table breaks down the key investment categories and their corresponding ROI metrics. This analysis provides a framework for building a comprehensive business case.
Total Cost of Ownership Analysis
Complete financial breakdown of implementation costs, ongoing expenses, and measurable ROI factors for medical voice recognition software
| Investment Category | Initial Implementation | Annual Ongoing | Hidden Factors | ROI Metrics | Payback Timeline |
|---|---|---|---|---|---|
| Software & Licensing | License fees, one-time purchase | Subscription fees, user additions | Per-user vs. enterprise license models | Direct cost savings from transcription | 12-24 months |
| IT Integration | EHR/EMR integration, API setup | Vendor support contracts, security audits | Custom workflow development costs | Increased revenue from accurate coding | 18-36 months |
| Hardware & Infrastructure | High-quality microphones, server upgrades | Network maintenance, cloud storage fees | Device compatibility and replacement cycle | Reduced claim denial rates | 18-36 months |
| Personnel & Training | Staff training sessions, onboarding | Continuous education, super-user programs | Physician productivity dip during learning curve | Decreased physician overtime, lower burnout | 6-12 months |
| Strategic Overhead | Project management, change management | Compliance monitoring (HIPAA) | Costs of poor user adoption | Improved physician retention, patient satisfaction | 24+ months (long-term) |
This table illustrates that the initial sticker price is only one part of the equation. A thorough evaluation must weigh the upfront and recurring costs against the quantifiable financial returns and strategic advantages, which often materialize over different time horizons.
Quantifying the Return: Beyond Time Savings
While reduced documentation time is a primary benefit, a compelling business case quantifies a broader range of financial returns. A major driver for adoption is the proven ability to significantly reduce administrative burdens, which directly impacts a practice's financial health. You can explore a deeper analysis of how AI voice agents can reduce administrative burden through various industry reports.
Successful organizations have measured ROI through:
- Reduced Transcription Costs: Many practices see a near-total elimination of third-party transcription service fees, often representing tens of thousands of dollars annually.
- Improved Coding Accuracy: High-quality, detailed notes captured by voice lead to more accurate medical coding and billing, reducing claim denials and increasing revenue capture.
- Decreased Physician Overtime: When physicians can complete their charts in real-time or shortly after a patient visit, it drastically cuts down on hours spent "pajama-timing" at home, reducing overtime pay and burnout.
- Strategic Benefits: While harder to quantify, benefits like higher physician retention and improved patient satisfaction scores due to more engaged clinicians have long-term financial value. Organizations should also consider the security benefits; our article on document management security highlights how robust systems protect valuable data.
The screenshot below from Nuance, a leading provider, shows various pricing tiers and packages, illustrating that vendors often structure costs based on features and scale.
This model allows organizations to select a plan that aligns with their budget and specific needs, from individual provider licenses to comprehensive enterprise agreements with ambient AI capabilities. By creating a detailed financial model that includes both the full spectrum of costs and a wide array of quantifiable benefits, you can build a powerful case for investing in medical voice recognition software.
Your Medical Voice Recognition Software Decision Framework
Translating an extensive analysis into a final decision requires a structured approach shaped by your specific healthcare environment. The best medical voice recognition software isn't a single platform that outperforms all others, but the one that aligns with your organization's distinct operational realities. This means prioritizing evaluation criteria based on what truly matters to your stakeholders—whether that's improving physician job satisfaction, reducing operational costs, or enhancing clinical quality outcomes.
Crafting Your Evaluation Roadmap
The first step is to establish a clear plan for vendor assessment and any pilot programs. This involves looking past marketing claims to focus on practical, real-world implementation factors. A successful evaluation should include:
- Stakeholder Alignment: Collect input from clinicians, IT staff, compliance officers, and administrative leaders. Each group holds different priorities, from user-friendliness to security protocols, and reaching a consensus early on is essential.
- Use-Case Definition: Clearly identify the primary problems you aim to solve. Are you targeting documentation time in a high-volume emergency department or seeking to improve note quality in a specialized outpatient clinic? The answer will direct your feature priorities.
- Vendor Negotiation Strategy: Enter discussions with a firm list of non-negotiable requirements, like specific EHR integration points or data residency rules. Understanding the market gives you a stronger position.
The medical speech recognition software market is expanding quickly. Detailed analysis projects its growth from approximately USD 1.68 billion in 2024 to around USD 5.32 billion by 2035. This growth, driven by demand for both cloud and on-premises solutions, points to a competitive field where vendors may be more flexible to secure strategic partnerships. You can review the complete medical speech recognition software market analysis to better understand these industry dynamics.
A Practical Decision-Making Guide
To simplify the selection process, this decision-tree infographic illustrates key branching points, from integration requirements to compliance readiness.
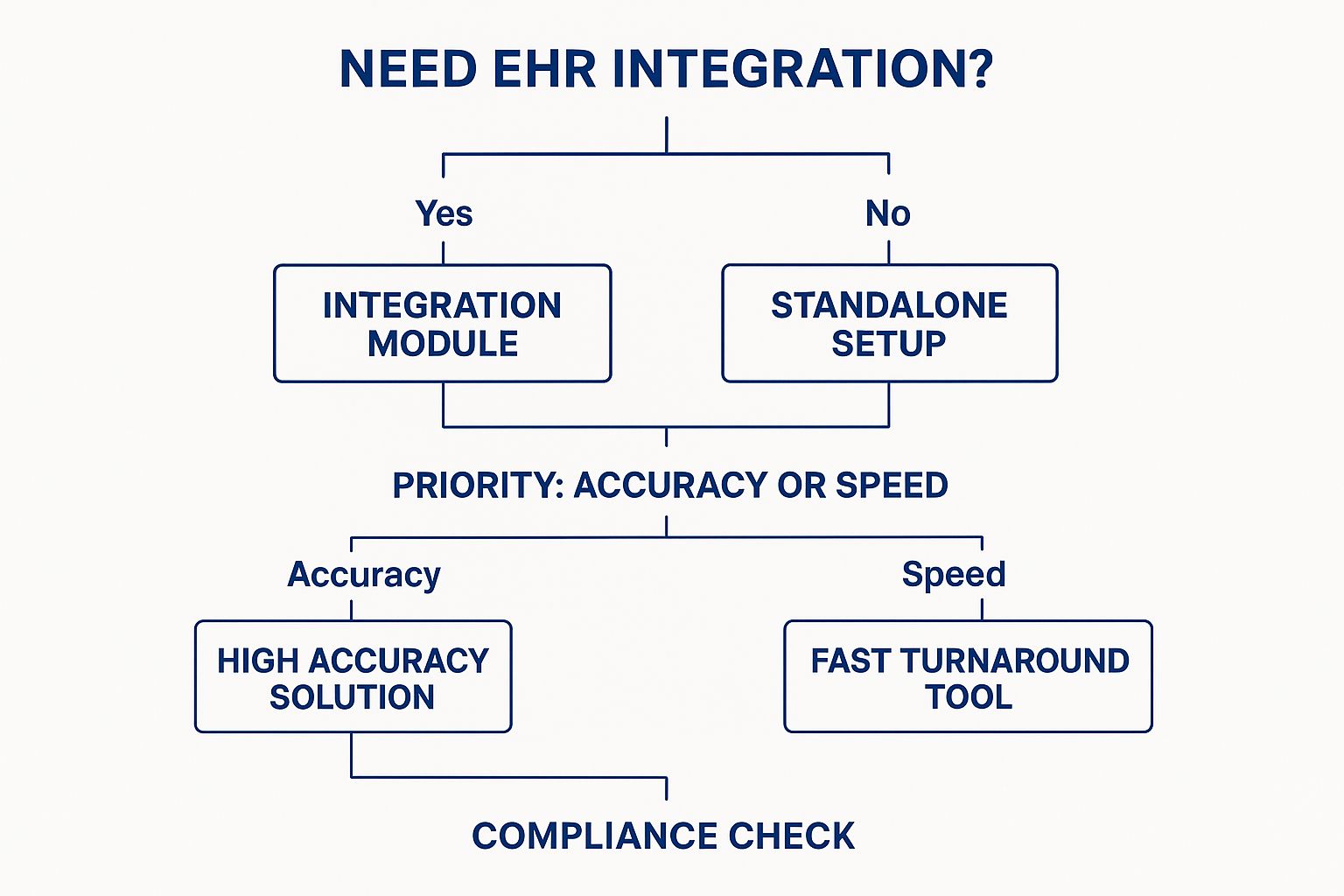
This visual guide demonstrates how initial technology needs—like EHR integration—and workflow priorities can steer you toward different types of solutions before you even start comparing specific vendors. The critical last step in this framework is ensuring your final choice satisfies all regulatory and security requirements.
For instance, federal bodies like HealthIT.gov provide extensive resources on certified health IT and data standards. Selecting software that adheres to established national standards is crucial for ensuring both interoperability and compliance.
As you move forward, remember that strong security measures are the foundation of any healthcare technology. To learn more, check out our guide on data security in healthcare. By following a structured framework, you can confidently choose a tool that fits your needs today and scales for the future.
If your priority is a secure, efficient, and privacy-focused dictation platform, Whisperit offers a powerful solution. Trusted by professionals in healthcare and other fields, Whisperit helps you complete documentation up to two times faster. Discover how our advanced AI can transform your workflow by visiting Whisperit.ai today.