Improving Clinical Documentation: Tips for Success in 2024
Understanding What Makes CDI Programs Actually Work
Improving clinical documentation isn't just about checking off requirements. It's about building a system that genuinely benefits patient care. Many healthcare leaders have successfully transformed their organizations by prioritizing documentation systems that actively support better outcomes, moving beyond simple compliance. The difference between thriving and failing Clinical Documentation Improvement (CDI) programs lies in understanding the core principles that set high-performing CDI teams apart.
One crucial element is a shift in documentation culture. Successful organizations engage physicians directly, creating smoother workflows and promoting lasting improvements. This collaborative approach ensures documentation standards not only lighten administrative burdens but also enhance clinical outcomes. For instance, some hospitals have successfully integrated concurrent review processes into existing clinical workflows, minimizing disruption and encouraging collaboration between CDI specialists and clinical staff.
Additionally, the clinical documentation improvement market has experienced significant growth. This expansion is fueled by factors like the transition to ICD-10 coding, demanding more detailed documentation. The global CDI market, valued at approximately $4.2 billion** in 2024, is projected to reach **$8.9 billion by 2034, representing a compound annual growth rate (CAGR) of around 7%. The rising use of Electronic Health Records (EHRs) further contributes to this growth by optimizing data capture and documentation practices, resulting in better revenue cycle management and fewer claim denials. For more insights, visit Future Market Insights.
Key Elements of a Successful CDI Program
Effective CDI programs share common characteristics. They focus on clear communication between CDI specialists and clinical staff, making sure everyone is aligned. They also use feedback systems that drive continuous improvement without adding unnecessary administrative overhead. This constant feedback loop allows the documentation process to adapt to the changing needs of the healthcare setting. For further reading, check out this article: How to master clinical documentation improvement.
These programs recognize the importance of accurate documentation but understand it shouldn’t compromise efficiency. They implement focused quality assurance processes to minimize errors while maintaining a streamlined workflow. By incorporating these key elements, CDI programs can substantially improve both the quality of patient care and the overall efficiency of healthcare operations.
Proven Strategies That Actually Improve Documentation Accuracy
Improving clinical documentation accuracy isn't simply about avoiding financial penalties. It's fundamentally about ensuring the delivery of the best possible patient care. This means putting into practice effective strategies that identify and address documentation gaps before they negatively impact patient outcomes or revenue streams. What techniques do successful healthcare organizations use to achieve this?
Concurrent Review and Clinical Workflow Integration
High-performing hospitals recognize the importance of integrating concurrent review processes seamlessly within existing clinical workflows. This integrated approach allows for the identification of documentation issues in real-time, minimizing disruptions to clinicians and facilitating immediate corrections. For example, integrating automated query workflows within the Electronic Health Record (EHR) system can streamline communication between Clinical Documentation Improvement (CDI) specialists and physicians, leading to faster resolution of documentation queries.

Fostering Communication and Collaboration
Robust communication protocols are essential for cultivating a collaborative environment between CDI specialists and clinical staff. Clear, respectful communication channels, combined with regular feedback mechanisms, create a shared sense of responsibility for documentation quality. This shared ownership is key to ensuring that documentation improvements are sustained over time. For more insights, read our article on How to Master Clinical Documentation Improvement Tips.
Targeted Quality Assurance Processes
Many organizations have seen a significant decrease in documentation errors through the implementation of targeted quality assurance processes. These processes may involve regular audits of medical records, with a focus on specific documentation elements or high-risk areas. Providing clinicians with real-time feedback and education on documentation best practices can further enhance accuracy.
Templates and Guidelines for Efficient Capture
Providing standardized templates and clear documentation guidelines not only supports accurate data capture but also promotes efficiency. Well-designed templates prompt clinicians for all necessary information, ensuring complete and consistent documentation across the entire organization. This approach improves data quality and saves valuable clinician time.
Building a Culture of Continuous Improvement
Finally, thriving CDI programs prioritize a culture of continuous improvement. This involves regularly analyzing documentation metrics, identifying areas for enhancement, and implementing data-driven changes. By actively monitoring progress and adapting strategies as needed, healthcare organizations can ensure the long-term efficacy and success of their CDI initiatives. For further information, you might be interested in our article on How to Master Clinical Documentation Improvement.
Smart Technology Integration for Better Documentation
The most successful healthcare organizations are strategically integrating new technology to improve their clinical documentation processes. This approach shifts documentation from a reactive task to a proactive way to improve patient care and operational efficiency. Let's explore the practical applications of AI and advanced documentation tools, examining how these technologies deliver tangible results.
AI-Powered Documentation Assistance
One key application is AI-powered documentation assistance, which learns from an organization's specific workflows. Imagine software that adapts to your processes, anticipating needs and streamlining tasks. This intelligent assistance offers features like automated coding suggestions and real-time feedback on documentation quality, going beyond simple transcription. This empowers clinicians to focus more on patient care and less on administrative work. You might be interested in: Our guide on medical speech-to-text software.
Natural Language Processing for Improved Clinical Note Quality
Natural language processing (NLP) is enhancing the quality of clinical notes. NLP algorithms analyze text to identify potential inconsistencies, missing information, and areas for improvement. This ensures greater accuracy and helps standardize documentation practices across the organization. Clinical notes become more comprehensive, consistent, and ultimately, more useful for both patient care and internal analysis.
Automated Coding Suggestions for Accuracy and Efficiency
Automated coding suggestions support both accuracy and efficiency. By analyzing clinical notes and suggesting appropriate codes, these tools minimize coding errors and reduce the time spent on manual code entry. This proactive approach helps ensure accurate billing and minimizes claim denials, contributing to better revenue cycle management. The integration of AI into CDI (Clinical Documentation Improvement) solutions is a key driver of this improvement, automating documentation processes and improving data quality. The increased use of telemedicine and precision medicine requires even more advanced documentation practices, increasing the need for sophisticated CDI solutions. Learn more about these market trends here.
Evaluating and Implementing Technology Effectively
Choosing the right technology is just the first step. Successful implementation requires careful planning and collaboration between IT professionals and clinical staff. Organizations should evaluate documentation technologies based on their specific needs, focusing on features that improve workflow and patient outcomes. This collaborative approach ensures that technology acts as a support system, not an additional burden.
Building CDI Teams That Drive Real Results
The success of a Clinical Documentation Improvement (CDI) program relies heavily on the team's strength. Building a team capable of driving real, lasting change requires the right people and the right support. It's about moving beyond simple compliance checklists and creating a team that can meaningfully improve clinical documentation.
Recruitment Strategies: Finding the Right CDI Specialists
Effective recruitment involves looking beyond basic qualifications. When searching for CDI specialists, prioritize candidates with strong analytical skills, extensive medical knowledge, and—crucially—the ability to collaborate effectively with clinical staff. This collaborative approach cultivates a shared responsibility for documentation quality, leading to more sustainable improvements. A strong team starts with individuals who are not only skilled but also possess the interpersonal skills to navigate the complex healthcare environment.
Essential Competencies for CDI Specialists
Effective CDI directors understand the importance of specific competencies. A strong understanding of medical terminology and coding guidelines is essential, along with proficiency in using Electronic Health Record (EHR) systems. Equally important, however, are soft skills such as communication, diplomacy, and the ability to educate and persuade. This blend of technical expertise and interpersonal skills allows CDI specialists to effectively connect clinical practice with documentation requirements. Check out our guide on workflow automation in healthcare.

Structuring CDI Teams for Maximum Impact
The ideal team structure depends on the organization’s size and complexity. Some hospitals embed dedicated CDI teams within specific clinical departments, while others use a centralized model. Regardless of structure, clear roles, responsibilities, and reporting lines are vital for accountability and efficiency. This clarity ensures everyone understands their contribution to the CDI program's overall success.
Ongoing Education and Mentorship
Continuous professional development is key for a high-performing CDI team. Regular training keeps staff updated on the latest coding guidelines and documentation best practices. Mentorship programs, pairing experienced CDI specialists with newer members, accelerate skill development and foster a supportive team environment. This investment in education and mentorship allows the team to adapt to evolving documentation needs.
Performance Metrics That Reflect Meaningful Outcomes
While tracking query rates and coding accuracy is important, effective CDI programs measure their impact on broader organizational goals. Relevant metrics might include case mix index accuracy, reduced claim denials, and improved patient outcomes. By focusing on these larger outcomes, CDI teams demonstrate their value in enhancing healthcare quality and efficiency. This data-driven approach enables continuous improvement and ensures the CDI program aligns with the organization’s strategic objectives.
Measuring Success Beyond Basic Metrics
Successful Clinical Documentation Improvement (CDI) programs go beyond simple checklists. They focus on tangible improvements in patient care and organizational performance. This requires looking past basic metrics to understand the true value created. How can we measure this deeper impact?
Key Performance Indicators for CDI Success
Effective CDI programs track key performance indicators (KPIs) that provide real insight into their effectiveness. This means moving beyond surface-level measurements and focusing on meaningful outcomes. For example, instead of just tracking query rates, these programs analyze how queries lead to more accurate diagnoses and better patient care.
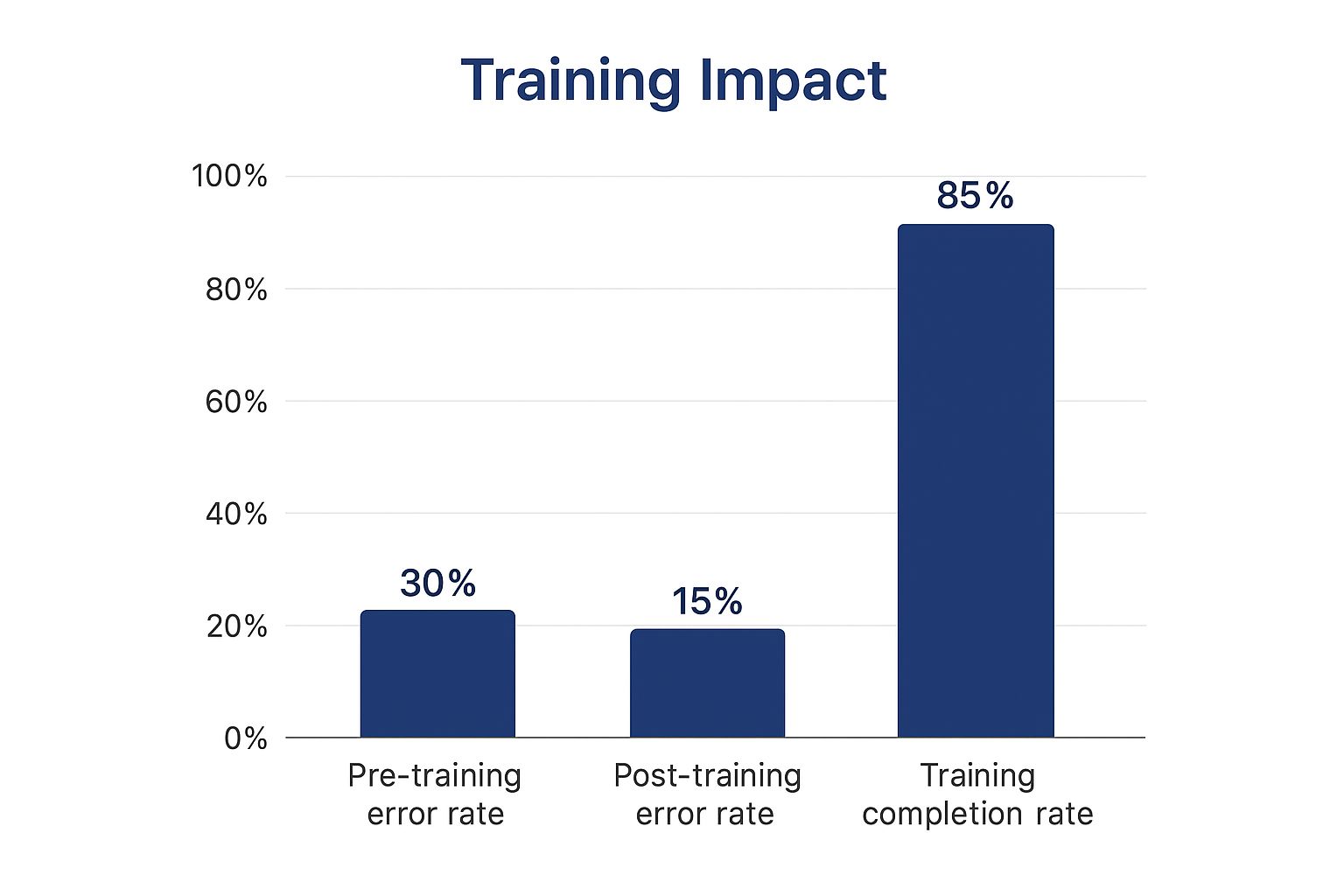
This infographic shows how training impacts documentation quality. The post-training error rate dropped significantly, combined with a high training completion rate. This points to successful staff education and positive improvements in clinical documentation. For further information, see our documentation review checklist.
Establishing Meaningful Baselines and Tracking Progress
To accurately measure progress, establishing meaningful baselines is essential. High-performing organizations analyze their current documentation practices before implementing any changes. This provides a clear starting point for measuring improvements, enabling data-driven decisions and highlighting areas where the CDI program is most effective. This data also helps communicate the program's value to stakeholders.
Communicating Results and Building Stakeholder Support
Communicating results clearly is vital for ongoing support. Presenting data that emphasizes the positive impact on patient care and financial performance can secure buy-in from physicians, administrators, and other key stakeholders. This transparent communication builds trust and reinforces the CDI program's value. For instance, demonstrating how improved documentation has resulted in more accurate reimbursement showcases the program's financial benefits.
The following table summarizes some key CDI performance metrics and benchmarks for healthcare organizations. It provides a comparison of essential metrics, their typical benchmarks, and how often they should be measured. The table also indicates the potential impact level of each metric on overall CDI program success.
Key CDI Performance Metrics and Benchmarks
| Metric | Industry Benchmark | Measurement Frequency | Impact Level |
|---|---|---|---|
| Query Rate | 5-10% of discharges | Monthly | Medium |
| Case Mix Index (CMI) | Varies by facility type | Quarterly | High |
| Denial Rate | < 5% | Monthly | High |
| Physician Query Response Rate | > 80% | Monthly | Medium |
| Coding Accuracy | > 95% | Quarterly | High |
This table provides a general overview. Specific benchmarks may vary based on individual facility characteristics and goals. Regular monitoring and analysis of these metrics are crucial for continuous improvement and demonstrating the effectiveness of the CDI program.
Calculating Return on Investment (ROI)
Calculating ROI accurately requires considering both direct and indirect benefits. While direct financial benefits, such as reduced claim denials, are easy to quantify, the indirect value of improved patient outcomes and increased physician satisfaction shouldn't be ignored. This comprehensive approach to ROI provides a complete view of the CDI program's impact. Demonstrating a clear ROI also helps secure resources and justify continued investment, ensuring long-term sustainability.
Using Data Analytics for Continuous Improvement
Successful CDI programs use data analytics to identify areas for improvement and optimize their strategies. Regularly analyzing documentation metrics pinpoints areas needing further training or process adjustments. This data-driven approach allows the CDI program to adapt to the changing healthcare environment, ensuring it continues to deliver results.
Choosing CDI Solutions That Actually Fit Your Needs

The market for Clinical Documentation Improvement (CDI) solutions offers a wide array of choices, ranging from sophisticated software platforms to specialized consulting services. Selecting the right fit for your healthcare organization requires careful planning and consideration. Each organization has unique characteristics in terms of size, complexity, and objectives.
This means a one-size-fits-all approach is rarely effective when choosing a CDI solution. How can you determine the optimal choice for your particular needs?
Evaluating Vendor Capabilities and Implementation Requirements
A critical step is thoroughly evaluating vendor capabilities, going beyond the initial sales presentations. This involves in-depth research of potential vendors, scrutinizing their track record, and obtaining feedback from their current clients. Understanding the implementation requirements is equally important.
Vendors often underestimate the time and resources necessary for a successful implementation. Developing a realistic timeline for your CDI program deployment is crucial to minimize disruptions and ensure a smooth transition. Key factors to consider include staff training, system integration with existing infrastructure, and the level of ongoing support provided by the vendor.
Tailoring CDI Strategies to Specific Needs and Budget Constraints
Successful healthcare organizations tailor their CDI strategies to align with specific regulatory requirements and budget limitations. They understand that improving clinical documentation is not just about compliance. It also significantly impacts patient care and overall organizational outcomes. The CDI market is broadly segmented into solutions and services, with the solutions segment taking a leading role in recent years.
In 2023, the solutions segment generated $2.7 billion in revenue, with a projected compound annual growth rate (CAGR) of 7.2%. The healthcare providers segment dominated the market by end-user, holding a substantial 68.7% share in 2023. This underscores the growing importance of CDI in healthcare settings. Learn more about market segmentation in the Clinical Documentation Improvement (CDI) Market report.
CDI Solutions vs. Services: Finding The Right Balance
The most effective approach often involves a combination of solutions and services. Some organizations choose to partner with consulting firms for the initial CDI program development and implementation, later transitioning to software solutions for ongoing maintenance and support. Other organizations prefer a hybrid approach, leveraging software for certain tasks while relying on consultant expertise for others. This flexibility allows for a customized CDI program that addresses the organization's unique requirements.
To help illustrate the different approaches, the following table provides a comparison of CDI solutions and services:
CDI Solutions vs Services Comparison: Detailed comparison of CDI solutions and services including features, costs, implementation time, and best use cases
| Approach | Key Features | Implementation Time | Best For | Average Cost Range |
|---|---|---|---|---|
| CDI Software | Automated query workflows, real-time feedback, data analytics | Varies depending on system complexity | Organizations seeking to automate CDI processes and improve efficiency | $50,000 - $500,000+ per year |
| CDI Consulting Services | Expert guidance on program development, implementation, and optimization | Varies depending on project scope | Organizations needing specialized expertise and support for CDI program launch or improvement | $500 - $2,000+ per day |
| Hybrid Approach | Combines software and services for a customized solution | Varies | Organizations seeking a flexible and tailored approach to CDI | Varies |
This table summarizes the key distinctions between using CDI software, engaging consulting services, or adopting a hybrid model.
By carefully evaluating these options, healthcare organizations can make well-informed decisions and select the approach that best aligns with their individual needs and resources. Investing in the right CDI solution ultimately translates to improved documentation accuracy, enhanced patient care quality, and stronger organizational performance.
Building CDI Programs That Last
The healthcare industry is in constant flux, requiring Clinical Documentation Improvement (CDI) strategies to remain adaptable and scalable. Organizations with a focus on the future are developing documentation programs that address both present needs and upcoming obstacles. This includes understanding emerging trends, from value-based care to population health management, and weaving them into a flexible CDI framework.
Adapting to Emerging Trends in Healthcare
Staying ahead of the curve involves anticipating what lies ahead for clinical documentation. Value-based care, for instance, prioritizes positive patient outcomes over the quantity of services provided. This requires detailed and thorough documentation to accurately reflect the complexities of patient care. Similarly, the increasing emphasis on population health management demands reliable data collection and analysis, underlining the need for standardized and precise documentation.
Building Flexibility into CDI Programs
Healthcare leaders are seeking strategies to build flexibility into their CDI programs while maintaining current operational effectiveness. This includes developing adaptable governance structures capable of responding to changing regulations and evolving industry best practices. One effective approach is forming a CDI steering committee composed of members from various clinical departments, ensuring alignment with the organization's overall strategic objectives. Such a committee also creates a platform for open dialogue and adaptation as new challenges arise.
Establishing Strong Partnerships for Long-Term Success
Thriving organizations recognize the value of collaboration. Cultivating strong partnerships with key stakeholders, such as physicians, coding professionals, and IT personnel, is vital for sustained CDI success. These collaborative relationships promote open communication and shared responsibility for documentation quality. Furthermore, they ensure the CDI program remains integrated with the organization’s established workflow.
Maintaining Staff Engagement Through Periods of Transition
Navigating change effectively can be difficult. Maintaining staff engagement during periods of transition is paramount. This requires providing ongoing training and consistent support to equip CDI specialists with the skills and knowledge necessary to thrive in a dynamic environment. It also involves fostering a culture of continuous improvement where staff are encouraged to identify areas for program enhancement.
Focusing on Patient Care Quality
Ultimately, patient care quality remains the top priority. Improving clinical documentation is not merely an administrative function—it has a direct impact on patient outcomes. By ensuring documentation is accurate, comprehensive, and readily accessible, CDI programs contribute to better clinical decision-making and enhanced patient safety. This patient-centric approach promotes a culture of quality improvement across the organization. By creating adaptable, collaborative, and patient-focused CDI programs, healthcare organizations can position themselves for long-term success in the ever-evolving healthcare landscape.
Ready to optimize your clinical documentation and improve your workflow? Learn more about how Whisperit can benefit your organization at https://whisperit.ai