How to Write a Medical Report: Expert Tips & Guide
Let’s be honest—writing a good medical report feels like a tightrope walk. You're balancing clinical precision, clarity for your colleagues, and the relentless pressure of the clock. So, what separates a decent report from an exceptional one? It’s all about crafting a structured clinical narrative that blends objective data with your expert interpretation, often using a familiar framework like SOAP.
The Foundations of Effective Medical Reporting
A medical report isn't just administrative paperwork; it's the official story of a patient's care. Think of it as a legal document, a communication bridge for continuity of care, and a critical piece of the puzzle for insurance and billing. A vague or incomplete report can cause real problems—diagnostic errors, treatment delays, and even serious legal and financial fallout.
This skill is so crucial that it's become a massive industry in itself. The global medical writing market was valued at around USD 3.8 billion in 2022 and is expected to soar to USD 8.4 billion by 2030. That growth isn't just a statistic; it shows a clear and rising demand for high-quality, precise clinical documentation across the board.
Before we break down the individual sections, it's helpful to see how they all fit together. Here’s a quick overview of the key components you'll find in a standard medical report.
Key Components of a Standard Medical Report
| Section | Primary Purpose | Information to Include |
|---|---|---|
| Patient Details | To accurately identify the patient and provide essential demographic context. | Full name, date of birth, medical record number, contact information, gender. |
| History | To document the patient's story and relevant medical background. | Chief complaint, history of present illness (HPI), past medical/surgical history, medications, allergies. |
| Findings | To present objective data from the physical examination and diagnostic tests. | Vital signs, physical exam results, laboratory values, imaging interpretations. |
| Assessment | To synthesize the subjective and objective information into a clinical diagnosis. | Primary diagnosis, differential diagnoses, and the clinical reasoning behind them. |
| Plan | To outline the next steps for the patient's treatment and management. | Further tests, new medications, specialist referrals, patient education, follow-up instructions. |
Each of these sections builds on the last, creating a comprehensive and legally sound record of care.
Why Structure Is Non-Negotiable
A standardized format, like the SOAP method, does more than just organize your notes. It provides a logical framework that sharpens your clinical thinking and ensures every critical detail is included and connected. This structure is what turns a scattered collection of observations into a coherent, defensible clinical story that any other provider can pick up and immediately understand.
A great medical report does two things perfectly: it accurately records what happened and clearly explains what should happen next. This dual function is the bedrock of safe and effective patient management.
This isn't about just ticking boxes. It’s about building a robust record of care that fully supports your clinical decisions. For a closer look at the specifics, you can review our guide on essential medical documentation guidelines.
Upholding Legal and Ethical Standards
Beyond clinical accuracy, every single report you write must comply with strict privacy and security rules. A huge part of effective reporting is knowing and following these regulatory guidelines.
For a thorough understanding of your obligations, it's essential to stay current on topics like HIPAA training requirements. Meeting these standards isn't optional—it’s a core professional duty that protects your patients, your practice, and you.
Capturing the Patient's Story Accurately

This is where the patient’s voice truly enters the report. The subjective section isn't just a list of symptoms; it's the clinical narrative. Getting this part right means skillfully documenting the Chief Complaint (CC), the History of Present Illness (HPI), and the relevant social and family history.
Your goal is to frame the patient's experience so clearly that any other clinician can understand the situation at a glance. You're setting the stage for everything that follows.
The Chief Complaint and History of Present Illness
Start with the Chief Complaint (CC). This should be a concise statement, ideally in the patient's own words, that cuts right to the heart of their visit. Think: "My chest feels tight, and I can't catch my breath."
From that single sentence, you expand into the History of Present Illness (HPI). This is the real story behind the CC. Instead of just noting "chest pain," use a structured approach like the "OLD CARTS" mnemonic to pull out the rich, relevant details.
- Onset: When did it start?
- Location: Where exactly is the symptom?
- Duration: How long has it been happening?
- Characteristics: What does it feel like—sharp, dull, aching?
- Aggravating/Alleviating Factors: What makes it better or worse?
- Radiation: Does the feeling move anywhere else?
- Timing: Is it constant or does it come and go?
- Severity: On a scale of 1 to 10, how bad is it?
Using a framework like this transforms a vague complaint into a detailed clinical account. It's an absolutely essential step in writing a medical report that leads to an accurate diagnosis.
Beyond the Immediate Problem
A truly thorough subjective summary goes deeper, including the patient’s past medical history, surgical history, family history, and social context. These pieces provide crucial context that can directly shape your assessment and plan.
For example, learning that a patient with new-onset shortness of breath has a family history of early-onset heart disease is a massive red flag. Likewise, understanding their social situation—maybe they live alone or work a physically demanding job—directly impacts your treatment and follow-up recommendations. It’s all about seeing the whole person, not just the symptom in front of you.
Capturing a detailed patient narrative isn’t just good practice; it's a diagnostic tool. The clues hidden in a patient’s story often point directly to the correct diagnosis long before any test results come back.
Of course, documenting this narrative is just one piece of the puzzle. For more insights on keeping this information structured and accessible, check out our guide on organizing medical records effectively. Proper organization ensures the rich details you gather don't get lost in a wall of text, making them easy to find and interpret for better patient outcomes.
3. Documenting Objective Data with Precision

Once you have the patient's story, it's time to shift to the hard data—the measurable, verifiable facts that form the "Objective" section of your report. This is where you document your physical examination findings, vital signs, and any available lab or imaging results. Think of it as the evidence that backs up your clinical reasoning.
The guiding principle here is to be relentlessly specific. Vague statements have no place in a quality medical report. I've seen too many notes with phrases like "lungs sound good" or "abdomen is soft." This kind of language isn't just imprecise; it’s clinically and legally indefensible. You’re aiming to create a clear, unambiguous record that any other clinician can understand and trust.
For instance, "lungs clear to auscultation bilaterally, no wheezes, rales, or rhonchi" paints a vivid clinical picture. "Lungs sound good" does not. This distinction is critical when you’re writing a report that needs to withstand scrutiny.
Organizing Your Findings for Clarity
From my experience, the most effective way to structure the objective section is by body system. A systematic, head-to-toe approach ensures you cover all the bases and makes the information easy for others to scan.
I always start with the fundamentals:
- Vital Signs: Get the numbers down—temperature, blood pressure, heart rate, respiratory rate, and oxygen saturation. I also make a quick note on whether the patient appears distressed or comfortable at rest.
- General Appearance: Add a few descriptive words about the patient's overall state. Are they "well-nourished" or do they "appear pale and fatigued"?
After that, I move methodically through each body system. Let's take a patient presenting with chest pain as an example. The notes might look something like this:
- Cardiovascular: Regular rate and rhythm, no murmurs, rubs, or gallops. Distal pulses are 2+ and symmetric. No peripheral edema.
- Pulmonary: Chest wall is non-tender to palpation. Good air entry bilaterally. Lungs are clear to auscultation.
- Gastrointestinal: Abdomen is soft, non-tender, non-distended. Bowel sounds are present and normal.
Pay close attention to the use of pertinent negatives. These are the findings that are absent but directly relevant to the chief complaint. For that patient with chest pain, noting "no peripheral edema" is just as important as documenting the heart rhythm.
Key Takeaway: Precision in this section is everything. Your objective findings are the factual bedrock of the entire report. They directly inform your assessment and justify your treatment plan, leaving no room for dangerous ambiguity.
To get this level of detail down quickly and accurately, many of us have found great success with tools like AI for medical transcription. These tools can capture your dictated notes with incredible accuracy, ensuring all the specific terminology you use is recorded perfectly. The journey of improving clinical documentation is a continuous one, and the right tech can make a massive difference in both quality and speed. This section isn't just about listing data; it's about presenting facts in a structured, logical, and defensible way.
Putting the Pieces Together: Crafting a Clear Assessment
This is where all your hard work comes together. The assessment is the analytical heart of your report, where you connect the dots between what the patient told you and what your examination revealed. Think of it as the moment you show your clinical reasoning. You aren't just dropping a diagnosis; you're building a clear, defensible argument for it.
A well-crafted assessment acts as a logical bridge from the history and findings to the plan you're about to outline. It justifies every test you order and every medication you prescribe. It's also the section that gets the most scrutiny for billing and coding, so getting it right is crucial. Any vagueness here can quickly turn into claim denials or compliance headaches.
Building and Justifying Your Diagnosis
For most encounters, your assessment will center on the primary diagnosis. But often, it’s more of a differential diagnosis—a ranked list of possibilities, from most likely to least likely.
The trick is to articulate why you've ranked them that way. Show your thought process.
- Top of the List: Directly link the patient's story and your objective findings to your primary conclusion. For instance, "Given the acute onset of exertional chest pressure radiating to the jaw and ST-segment elevation on the EKG, the working diagnosis is an acute myocardial infarction."
- Other Possibilities: Briefly touch on why other conditions are still in the running, even if they're a long shot. Something like, "Pulmonary embolism is also a consideration due to the sudden dyspnea, though the absence of pleuritic pain or tachycardia makes it less likely."
- Ruled-Out Conditions: It's good practice to mention any serious conditions you've confidently excluded based on what you found (or didn't find).
This approach tells any other provider who reads your note exactly what was on your mind. That level of detail is a pillar of strong clinical documentation improvement, reinforcing the report's value both clinically and for administrative purposes.
Navigating Diagnostic Uncertainty
It’s completely fine—and often the reality—to have a working diagnosis when a definitive one isn't yet possible. The important thing is to be upfront about that uncertainty. Using phrases like "probable," "suspected," or "unexplained" clearly signals that your assessment is preliminary and subject to change as more data comes in.
The assessment isn’t just a conclusion; it’s a transparent display of your clinical judgment. It needs to logically explain how you arrived at your diagnosis and justify the plan that follows.
This kind of precision is becoming a global standard. For example, the medical writing market in the Asia-Pacific region is expanding at over 11% CAGR, largely because new regulations demand more clarity in clinical documentation. This trend highlights a universal need for medical reports that are both precise and well-justified. You can read more about what's driving this growth in this market analysis.
Crafting a Specific and Actionable Plan
We’ve arrived at the final, and arguably most crucial, part of the report: the "Plan." Think of it as the road map for your patient's care. If the assessment answers what you believe is going on, the plan lays out exactly what you're going to do about it. This section is what turns a static document into a dynamic tool that directly influences patient outcomes.
Vague plans are a recipe for confusion and poor follow-through. You’ve probably seen them before—phrases like "follow up as needed" or "start medication." They're not enough. Every single step needs to be specific, measurable, and clearly tied back to a problem you identified in the assessment. This level of clarity is vital for continuity of care, making sure any colleague can pick up where you left off without missing a beat.
This visual shows how all the pieces of your report logically flow into these final recommendations.
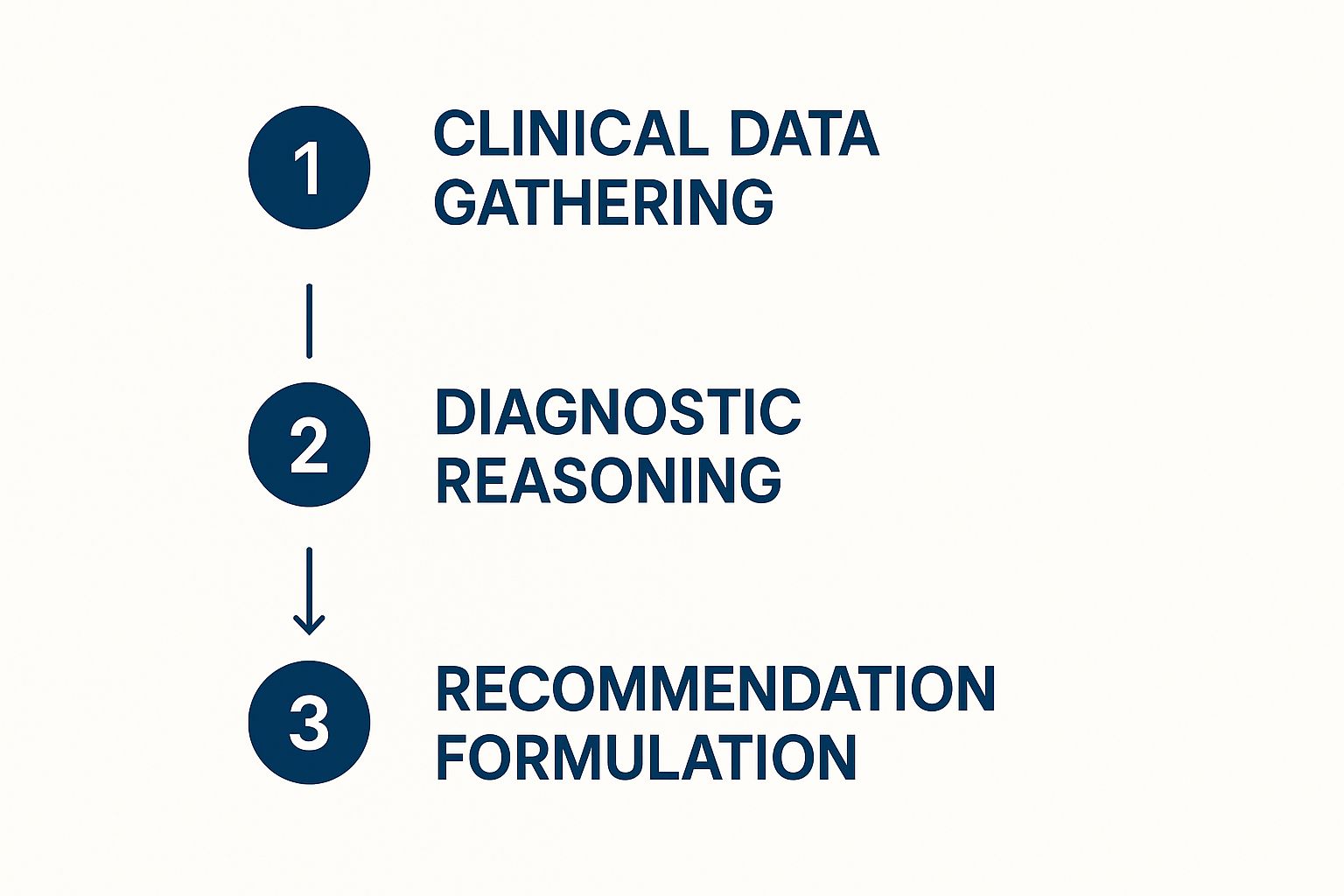
As you can see, the plan isn't an afterthought. It’s the direct result of methodical data gathering and sharp diagnostic reasoning.
How to Structure an Effective Care Plan
From my experience, the most effective way to structure the plan is with a numbered list. Each number should correspond directly to a specific diagnosis or problem from your assessment section. This one-to-one mapping is a simple but powerful way to ensure nothing falls through the cracks.
Let’s walk through an example. For a patient with newly diagnosed hypertension and hyperlipidemia, a solid plan would look something like this:
- Hypertension:
- Initiate Lisinopril 10 mg by mouth, once daily.
- Patient to get a home blood pressure cuff and log readings twice a day for the next two weeks.
- Discussed the benefits of a low-sodium diet and gave the patient an educational handout.
- Hyperlipidemia:
- Start Atorvastatin 20 mg by mouth, to be taken once daily at bedtime.
- We’ll recheck the lipid panel in 3 months to see how well it's working.
- Provided counseling on lifestyle changes, emphasizing increased physical activity.
- Follow-Up:
- Schedule a return visit in 4 weeks to go over the blood pressure logs and check for any medication side effects.
This level of detail leaves no room for guessing games. It spells out the "what" (medication, test), the "how much" (dosage), and the "when" (frequency, follow-up).
A truly actionable plan does more than just list treatments. It establishes a clear timeline and sets expectations for both the patient and any other providers involved. This kind of proactive management is a hallmark of high-quality care.
This clarity has practical benefits beyond the clinical, too. Unclear care plans can lead to billing snags and even medical debt if patients aren't clear on their options. A well-documented plan provides justification for procedures and can be a tool to guide patients toward necessary resources.
Weaving In Patient Education and Referrals
A truly complete plan must also account for patient education. Always document that you've discussed the diagnosis, the "why" behind your treatment choice, and any potential side effects. This is a core part of informed consent.
Be just as specific with your referrals. "Refer to Cardiology" is okay in a pinch, but "Refer to Cardiology for stress testing and further management of coronary artery disease" is infinitely better. It gives the consulting physician immediate context.
Getting this detailed documentation style down is a skill that pays dividends. If you're looking to sharpen your abilities, our guide on medical transcription training provides foundational knowledge that will improve your reporting accuracy and speed. Ultimately, a clear and actionable plan is the final, essential step in crafting a medical report that truly makes a difference.
Common Questions About Medical Reporting
Even when you know the rules, the reality of creating medical reports day in and day out brings up some practical questions. I've been there. Let's tackle a few of the most common hurdles clinicians run into, with some straightforward advice to help you fine-tune your documentation and sidestep potential issues.
How Can I Make My Reports More Concise?
We all struggle with this. The key is to shift from conversational language to precise, active terminology. For instance, instead of a lengthy "The patient told me that they have been experiencing significant pain in their left knee," a much cleaner "Patient reports left knee pain" communicates the exact same information. It's direct and professional.
Another trick I've picked up is using formatting to your advantage. Don't bury a long list of medications or past surgeries in a dense paragraph.
- Break them out into bullet points.
- This makes the report instantly scannable for colleagues or specialists who need to find that information fast. You lose zero detail but gain a ton of clarity.
What Are the Biggest Legal Risks with Poor Reporting?
Frankly, the risks are significant and can't be understated. Poorly written reports can quickly lead to malpractice claims built on miscommunication. They can also trigger accusations of billing fraud if your documentation doesn't support your coding. And of course, there's always the risk of breaching patient privacy.
Your report is the definitive legal record of care. Think of it this way: a clear, objective, and timely report is your single best defense if a question ever arises.
A well-written medical report is more than just a clinical tool; it's a legal shield. Its clarity and accuracy directly protect you, your facility, and your patient from preventable harm and legal challenges.
What Is the Best Way to Correct an Error?
The golden rule is transparency. Never, ever try to delete, white-out, or otherwise obscure the original entry. The standard and correct way is to draw a single, clean line through the mistake, write "error," and then add your initials and the date. Right after that, you add the correct information.
This process is even more structured within an electronic health record (EHR). Don't just try to edit the text. Always use the system's official function for creating an addendum. This creates a clear, time-stamped audit trail that preserves the integrity of the patient's record.
Ready to make your documentation faster, smarter, and more secure? Discover how Whisperit can help you complete reports in half the time with advanced AI dictation and customizable templates. Visit our site to learn more about how it works.