A Guide to Healthcare Technology Solutions
Healthcare technology solutions aren't just about fancy gadgets or complicated software. At its heart, this is all about using digital tools to solve real-world problems in medicine—making patient care better, helping hospitals run smoother, and ultimately, improving people's health.
Think of everything from the digital charts your doctor uses (EHRs) to the AI that can help a radiologist spot a tiny tumor on a scan. It’s technology applied with a clear purpose: to overcome the daily hurdles that get in the way of great medical care.
How Healthtech is Reshaping Modern Medicine

Picture a hospital where information moves effortlessly. A patient’s lab results pop up instantly in their digital chart. Their family doctor and a specialist in another city can both look at that same chart, at the same time, to decide on the best treatment. That’s the promise of modern healthtech in a nutshell: seamless coordination, accuracy, and efficiency.
These aren't just pie-in-the-sky ideas. They're practical tools built to fix problems that have plagued healthcare for decades, like siloed patient data, mountains of administrative work, and the simple difficulty of getting care when you need it. Technology tackles these issues head-on by building a smarter, more connected healthcare environment.
Why Technology Isn't Just "Nice to Have" Anymore
The push for technology in healthcare is coming from a real need to work smarter and deliver better results for patients. It’s why health plan leaders consistently put modernizing their tech at the top of their to-do lists. They know that by replacing clunky, old systems, they can make their organizations more nimble and secure.
So, what are the big goals here?
- Making Care Safer: When you reduce manual data entry and give a doctor a patient's complete medical history in seconds, you cut down on the risk of human error. It’s that simple.
- Getting Diagnoses Right: AI tools can scan medical images and patient data, picking up on subtle patterns the human eye might miss. This can lead to earlier, more accurate diagnoses.
- Opening Up Access to Care: Telehealth platforms are a game-changer. They connect people in remote areas with top specialists and just make healthcare more convenient for everyone.
The market growth tells the story. The global healthcare AI market is expected to grow at a staggering compound annual rate of 38.5% between 2024 and 2030. That’s a huge signal that the industry is all-in on building smarter tools.
At the end of the day, healthcare technology solutions give clinicians the freedom to focus less on paperwork and more on what truly matters: taking care of patients. This focus is the foundation for lasting healthcare quality improvement initiatives and is quickly becoming the new benchmark for excellence in medicine.
The Four Pillars of Modern Healthtech
When we talk about healthcare technology solutions, it's easy to get lost in a sea of acronyms and buzzwords. But it's much simpler if you think of it all as a single, coordinated system built on four distinct pillars. Each one has a specific job, but they’re all designed to work together, supporting a smarter, more connected, and patient-focused healthcare model.
Think of them as the foundational columns holding up a modern digital clinic. Let's break down what each one does and how it fits into the bigger picture.
Pillar 1: Electronic Health Records (EHRs)
At the very heart of digital health, you'll find Electronic Health Records (EHRs). These are so much more than just digital filing cabinets. A good EHR tells the complete, real-time story of a patient's health journey. It brings together everything—diagnoses, medications, lab results, allergies, immunization dates—into one secure and accessible place.
Picture this: a patient arrives at the ER, unable to communicate clearly. Instead of guessing, the doctor can pull up their entire medical history in seconds, spotting a critical allergy noted by their primary care physician months ago. This immediate access to information is a game-changer, drastically cutting down on medical errors and leading to faster, safer decisions. In essence, the EHR is the "single source of truth" for patient care.
Of course, just having an EHR isn't the whole story. The data inside needs to be clean, organized, and easy for clinicians to use. To learn more about getting the most out of these systems, check out our guide on electronic health record optimization.
Pillar 2: Telehealth and Remote Patient Monitoring
The second pillar, Telehealth, acts as a virtual bridge, completely dissolving the physical distance between patients and providers. It uses everyday technology, from video calls to smart at-home devices, to deliver care wherever the patient is. This isn't just about making appointments more convenient; it’s a fundamental change in how people access medical care.
Take a patient managing high blood pressure. With a connected blood pressure cuff at home, their daily readings are sent directly to their doctor. This constant stream of data, a practice known as Remote Patient Monitoring (RPM), allows the clinical team to spot worrying trends and step in before a crisis happens. It's proactive care that keeps people healthier and out of the hospital.
This infographic helps visualize how these pillars connect.
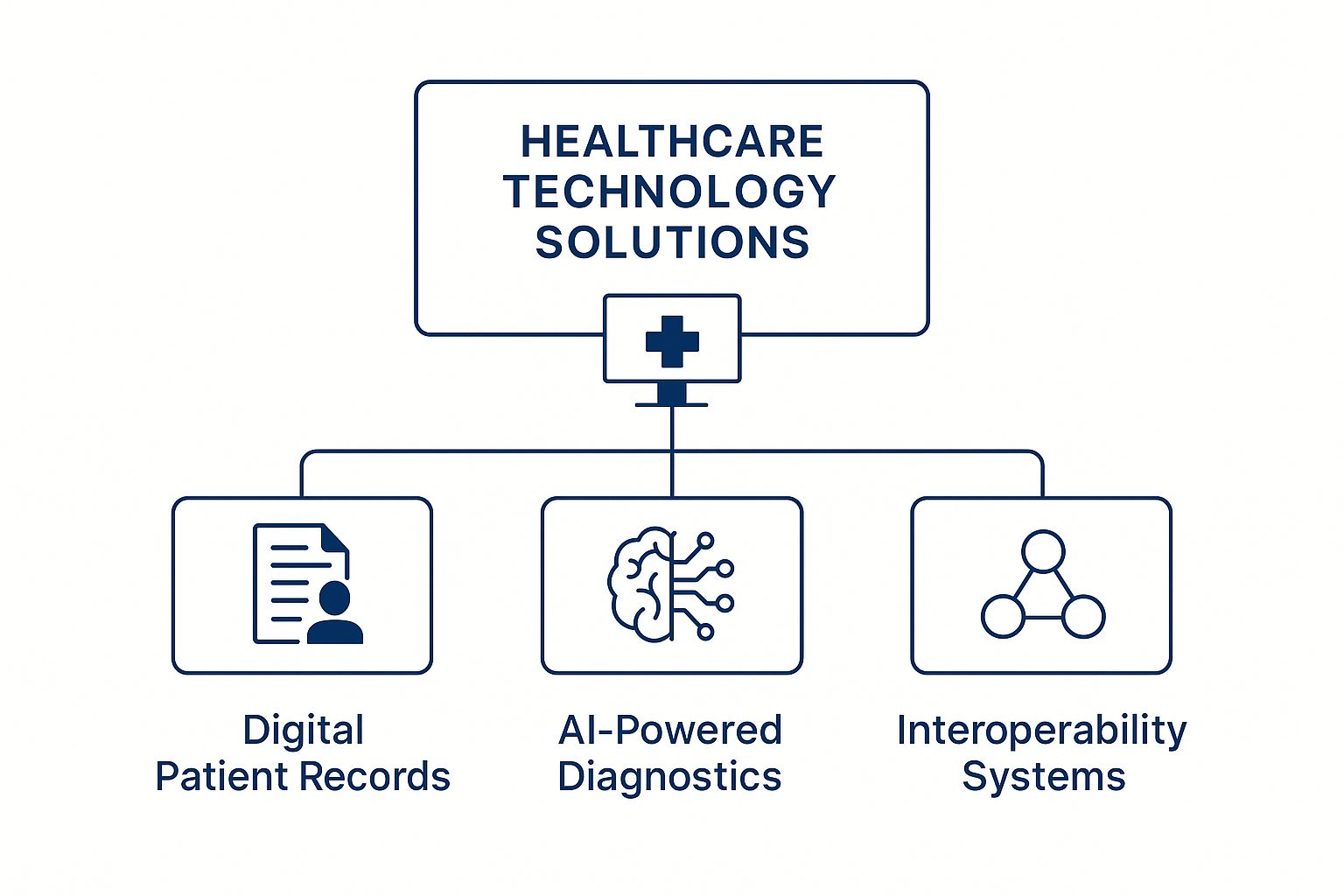
As you can see, foundational tools like EHRs are the bedrock for advanced applications like AI diagnostics, with interoperability being the essential glue holding it all together.
Pillar 3: Artificial Intelligence and Machine Learning
If EHRs are the healthcare system's memory, then Artificial Intelligence (AI) and Machine Learning (ML) are its brain. This pillar is all about using smart algorithms to dig through massive amounts of health data, find hidden patterns, and make predictions that can directly improve patient outcomes. AI is the engine that turns raw data into life-saving insights.
For instance, AI models can now analyze medical images like X-rays or CT scans with incredible accuracy, flagging tiny anomalies that the human eye might overlook. In another clinic, AI might be crunching patient data to identify individuals at high risk for developing a certain disease, enabling doctors to intervene early with preventative care. AI isn't about replacing doctors; it's about giving them superpowers.
Pillar 4: Interoperability Systems
The final pillar is Interoperability, and it might just be the most important one because it’s what makes everything else work together. Think of it as the universal translator for healthtech. Different hospitals, labs, and pharmacies all use different software, which often creates digital islands where patient data gets stuck. Interoperability builds the bridges between those islands.
It creates a common language that allows a hospital's EHR, a diagnostic lab's system, and a local pharmacy's software to talk to each other seamlessly. When a specialist adds a new medication to a patient’s file, interoperability ensures that update appears instantly and accurately in the primary care physician's system, too. Without it, a truly connected healthcare system would be impossible.
To pull this all together, here’s a quick comparison of how these four pillars function side-by-side.
Comparing the Four Pillars of Healthcare Technology
| Technology Pillar | Primary Function | Key Benefit for Providers | Example Application |
|---|---|---|---|
| Electronic Health Records (EHRs) | Centralizing all patient data in one digital record. | Immediate access to a complete patient medical history. | An ER doctor views a new patient's allergy list. |
| Telehealth & RPM | Delivering care and monitoring patients remotely. | Improved patient access and proactive chronic care management. | A cardiologist reviews at-home blood pressure readings. |
| AI & Machine Learning | Analyzing data to provide predictive insights and decision support. | Augmenting diagnostic accuracy and identifying at-risk patients. | An algorithm detects early-stage cancer on a CT scan. |
| Interoperability Systems | Enabling different software systems to share data seamlessly. | A unified view of patient information across care settings. | A hospital EHR automatically receives lab results from an external lab. |
Each pillar is powerful on its own, but when integrated, they create a healthcare infrastructure that is safer, smarter, and far more responsive to the needs of both patients and providers.
How AI Is Changing Patient Care

Artificial intelligence has officially moved out of the lab and into the clinic. It’s no longer just a buzzword but a practical, powerful tool that’s working alongside doctors and nurses. The real story here isn’t about replacing human expertise; it’s about amplifying it with data-driven insights. Think of AI as the sharpest instrument in the modern medical toolkit, helping to make care more precise, efficient, and proactive.
Picture a radiologist looking at a chest X-ray. An AI algorithm, which has learned from millions of other scans, is right there with them, flagging a faint shadow that might signal an early-stage tumor. This kind of collaboration leads to earlier intervention and, ultimately, much better outcomes for patients.
This blend of human skill and machine precision is where AI truly shines. It’s like having a tireless assistant that helps clinicians spot more details and act on them faster. It's easily one of the most impactful healthcare technology solutions we have today.
From Diagnostics to Documentation
AI's applications in healthcare are incredibly broad, touching almost every part of a patient's journey. From the moment of diagnosis to ongoing treatment and even the administrative work that follows, AI-powered tools are making a real difference.
One of the most obvious wins is in diagnostics. AI models are masters of pattern recognition, which makes them perfect for sifting through complex medical data. Here’s where they’re already making an impact:
- Medical Imaging: AI can analyze MRIs, CT scans, and X-rays to find subtle signs of diseases like cancer or diabetic retinopathy with astounding accuracy.
- Pathology: Algorithms are helping pathologists examine tissue samples on digital slides, identifying cancerous cells faster and more consistently than ever before.
- Genomics: By analyzing genetic data, AI helps pinpoint a person's risk for certain diseases, opening the door to truly personalized medicine.
For a deeper dive into how this works in practice, you can find great examples in this resource on AI for Medical Imaging and Diagnostics. The field is moving quickly, offering new hope for catching diseases earlier.
Beyond just finding problems, AI is also tackling the mountain of paperwork that contributes to clinician burnout. Ambient clinical intelligence systems can now listen to a doctor-patient conversation and automatically create accurate clinical notes in the background.
This is huge. It means doctors can finally put down the keyboard and focus completely on the person in front of them. By taking over this tedious task, AI hands back precious time for more meaningful patient conversations. If you're curious about how voice technology is driving this shift, you can learn more about the advances in medical speech recognition.
Personalizing Treatment and Predicting Outcomes
Another exciting frontier for AI is its ability to craft personalized treatment plans. We’re moving away from a one-size-fits-all approach. Instead, machine learning models can analyze a patient's unique genetic profile, lifestyle, and medical history to predict which therapies will work best for them.
This predictive power also helps identify patients who are at high risk for complications. For instance, an AI system can monitor real-time data from patients in a hospital and alert a nurse if someone is showing the earliest signs of sepsis, enabling a team to step in immediately.
AI's ability to process millions of data points allows it to forecast potential health events, shifting the focus from reactive treatment to proactive prevention. It helps answer the critical question: "What might happen to this patient, and how can we prevent it?"
This isn’t just a niche idea; it’s gaining serious traction. In Deloitte's 2025 Global Health Care Outlook, over 80% of health system executives said they believe generative AI will have a significant or moderate impact on their organizations by 2025. They see its potential everywhere, from diagnostics to day-to-day operations. This growing confidence shows that healthcare leaders now see AI not as a far-off concept, but as a core part of modern medicine.
Expanding Access with Telehealth and Remote Monitoring

Let's be clear: telehealth is much more than just a video call with your doctor. It's a complete shift in how we think about delivering healthcare, tearing down the geographic and logistical walls that have always separated patients from timely care. These healthcare technology solutions have become a virtual bridge, bringing expert medical care right into a patient's living room.
This isn't just for a quick check-in about a cold. We're talking about a powerful way to manage chronic conditions, deliver crucial mental health support, and handle urgent care needs without forcing someone to travel. For many people, especially those in remote areas or with mobility issues, this is the difference between getting consistent care and getting none at all.
Proactive Care with Remote Patient Monitoring
A huge piece of the telehealth puzzle is Remote Patient Monitoring (RPM). The best way to think about it is giving a doctor a window into a patient's daily health, long after they've left the clinic. Using simple, connected devices at home, patients can track their vital health data without even thinking about it.
This steady stream of real-world information paints a far more accurate picture of a person's health than a single, snapshot-in-time office visit ever could. It allows clinical teams to get ahead of problems, shifting from a reactive "fix-it-when-it's-broken" model to a truly proactive one.
- For Diabetes Management: A patient’s smart glucose meter automatically sends daily blood sugar readings straight to their endocrinologist.
- For Heart Conditions: A connected blood pressure cuff and weight scale can alert a cardiology team to the early warning signs of worsening heart failure.
- For Respiratory Illness: A pulse oximeter keeps a close eye on oxygen levels for a patient with COPD, enabling an intervention before their levels become dangerous.
This is all about spotting negative trends early. Clinicians can then adjust treatment plans before a small issue spirals into an emergency room visit, which is a game-changer for reducing hospital readmissions and improving long-term health.
Making Geography Irrelevant
Think about someone living in a rural town who needs regular appointments with a neurologist. In the past, that meant taking a whole day off work, driving for hours, and footing the bill for gas and time lost. It was a massive burden.
Now, that same person can have their follow-up appointments over a secure video call. The specialist can review data streaming in from their at-home monitoring devices, talk through symptoms, and tweak medications on the spot. An in-person visit might still be needed from time to time, but the day-to-day management of their condition happens from the comfort of home.
We often call this hybrid approach "phygital care." It’s the sweet spot that combines the convenience and data-rich insights of digital health with the irreplaceable human touch of traditional medicine. The result is a more flexible, patient-focused experience.
And this isn't just a futuristic idea—it's happening now. The global telehealth market is on track to blow past USD 55 billion by the end of 2025, showing just how fast this shift is accelerating. This incredible growth is fueled by undeniable benefits: better access to specialists, smarter management of chronic diseases, and putting patients back in control of their own health.
New Frontiers in Virtual Assessments
Telehealth is also breaking new ground in areas that were once strictly in-person, like initial diagnostic assessments. It’s creating a lifeline for specialized evaluations where distance or mobility would have previously been a showstopper.
For instance, the technology is playing a vital role in enabling accessible telehealth for autism diagnosis, which allows specialists to conduct detailed observations and family interviews remotely. This helps ensure that critical developmental assessments aren't put on hold simply because of where a family lives. Of course, documenting these virtual encounters properly is crucial, and knowing the specific telehealth documentation requirements ensures everything stays compliant. By knocking down these old barriers, telehealth is connecting more people to the specialized care they need, exactly when they need it.
A Practical Guide to Implementing Healthtech Solutions
Bringing new healthcare technology solutions into your practice can feel overwhelming, but with the right game plan, it's entirely manageable. A successful rollout is a delicate balance of the right tech, smart processes, and, most importantly, your people. Get it right, and you can energize your entire team and improve patient care. A rushed job, on the other hand, just creates headaches and disrupts the workflows you were trying to fix.
The whole journey starts way before you install a single piece of software. It kicks off with a simple question: What, exactly, are we trying to solve here? Without a crystal-clear answer, even the most impressive tech is just a shiny, expensive distraction.
Start with a Thorough Needs Assessment
First things first: you have to do a deep dive into your organization's specific challenges and goals. This isn't about chasing the latest shiny object. It’s about identifying the real, everyday pain points that are holding you back. Are your clinicians buried in administrative work? Are you struggling to keep tabs on patients with chronic conditions once they leave the office?
The only way to get real answers is by talking to the people in the trenches—your doctors, nurses, and front-desk staff. Their day-to-day experiences will point you directly to the biggest opportunities for improvement.
- Map Your Current Workflows: Get a clear picture of how things are done now. This will immediately highlight the bottlenecks and time-wasting steps.
- Define Clear Objectives: Be specific and set measurable goals. Are you aiming to cut patient wait times by 15%? Or maybe reduce documentation errors?
- Prioritize What Matters: Make a "must-have" vs. "nice-to-have" list for any new tool. This will keep you focused during the selection process.
Laying this groundwork ensures you end up with a solution that actually fits your needs, not just one that has a great sales pitch. It's the difference between buying a tool and truly solving a problem.
Manage the Human Side of Technology
Here’s a hard truth: the tech itself doesn't guarantee a win. It's all about user adoption. The biggest roadblock to any new implementation is almost always our natural resistance to change. That’s why a thoughtful change management plan is non-negotiable if you want your team to actually embrace the new tools.
This means doing more than just a one-off training session. You need to build a culture of support where your staff feels heard and gets the help they need to feel confident with the new system.
"The most successful healthtech implementations focus as much on the 'peopleware' as they do on the software. When clinicians are involved in the process and see how a new tool directly benefits their work and their patients, they become its biggest champions."
Open communication is everything. Explain the why behind the change. Show your team how it will make their lives easier—less paperwork, better patient insights, more time for what matters. Offer hands-on, role-specific training and pick a few tech-savvy "super-users" in each department who can act as go-to resources for their peers. When people feel empowered instead of forced, adoption happens naturally.
Focus on Data Migration and Integration
Once you’ve picked your solution and gotten your team ready, it’s time to get technical. Moving patient data from an old system to a new one, a process called data migration, is like performing surgery. It requires meticulous planning to make sure every piece of information is transferred accurately and securely.
Just as critical is integration. Your new technology has to play nicely with the systems you already rely on, like your EHR or billing software. A tool that operates in a silo and doesn't share data just creates more work, completely defeating the purpose. Before you sign anything, make sure your vendor can show you proof of successful integrations with systems just like yours. A seamless technical launch is the final, crucial step to unlocking the true value of your new healthcare technology.
Navigating Security and Compliance in Digital Health
As we rely more and more on healthcare technology, our responsibility to protect sensitive patient information grows right alongside it. This isn't just a technical checkbox; it's the very foundation of patient trust. Every single digital touchpoint, whether it's a quick telehealth check-in or a simple update to an electronic health record, handles data that must be kept secure, private, and compliant with some incredibly strict regulations.
Think of digital health security as the vault protecting a hospital's most valuable asset—its patient data. A breach isn't just a data leak; it's a deep violation of trust that can have devastating consequences for patients and the healthcare organization. And the threat is very real. With hundreds of healthcare cyber-attacks reported every year, strong security is simply not negotiable for any modern healthtech strategy.
Understanding HIPAA and Its Role
In the United States, the conversation around healthcare data protection always starts with the Health Insurance Portability and Accountability Act (HIPAA). The name is a mouthful, but its core purpose is straightforward: to set the national standard for protecting what's known as Protected Health Information (PHI). This covers everything from a patient's name and diagnosis to their insurance details.
HIPAA is more than just a list of rules; it's a blueprint for building a culture of security. It mandates that healthcare providers and their tech partners put specific safeguards in place to control exactly who can see and use patient data. For a clear, actionable guide on these duties, reviewing a HIPAA compliance requirements checklist is a great place to start.
Simply put, HIPAA ensures that patient information is used for providing care—and not for anything else. Compliance is the absolute baseline for any healthcare technology solution that hopes to be taken seriously.
Essential Security Measures in Healthtech
Protecting patient data demands a defense-in-depth strategy. It’s never about one single tool; it’s about a combination of practices and technologies all working in concert. It's no surprise that a staggering 46% of health plan executives now say security is their top priority for technology modernization—the urgency to get this right has never been greater.
Here are the cornerstones of a strong defense:
- Data Encryption: This is the process of scrambling patient data, turning it into unreadable code for anyone without the right key. It's like sending a message in a secret language that only the intended recipient can understand.
- Multi-Factor Authentication (MFA): This adds a crucial second layer of security on top of a password. It requires another form of verification, like a code sent to your phone, to prove you are who you say you are.
- Access Controls: This is all about making sure clinicians can only see the specific patient information they need to do their jobs—nothing more. A billing clerk, for instance, has no reason to see a patient’s detailed clinical notes.
By embedding these measures into their core design, healthcare technology solutions create a secure environment where data is protected at every step. That's why choosing vendors who build privacy and security into their products from the ground up isn't just a good idea; it's essential for maintaining compliance and the sacred trust between patients and their providers.
Answering Your Questions About Healthtech
Stepping into the world of healthcare technology brings up a lot of practical questions. You're probably wondering about the real-world costs, the headaches of implementation, and what all this means for the future of your practice. Let's tackle some of the most common questions we hear.
What's the Single Biggest Hurdle in Implementation?
You might think it’s the tech itself, but it’s almost always the people. The biggest challenge is change management.
Successfully introducing a new EHR or telehealth platform isn't just about flipping a switch. It requires getting your team on board, which means great training, constant communication about why this change is happening, and including your clinical staff in the decision-making process from the start. If you can’t get your team to adopt the new tools, you’ll never see the benefits.
Can a Small Clinic Actually Afford These Advanced Tools?
Yes, absolutely. The game has changed thanks to cloud-based, Software-as-a-Service (SaaS) models. This is a huge win for smaller practices.
Instead of a massive upfront investment in hardware and software licenses, clinics can now pay a predictable monthly subscription. This fee usually covers everything—updates, security, and tech support. It levels the playing field, giving smaller organizations access to the same powerful technology as major hospital systems without the crippling initial cost.
The future role of clinicians will be more focused on empathy, complex problem-solving, and managing the human side of care, enhanced by AI-driven insights.
Is AI Going to Replace Doctors?
Not at all. Think of AI as a powerful partner, not a replacement. Its real job is to augment what healthcare professionals do best.
AI is fantastic at handling the repetitive, administrative grunt work—things like transcribing notes, organizing data, and flagging potential issues in patient records. This automation frees up doctors and nurses to spend less time on their keyboards and more time face-to-face with patients.
It also acts as a brilliant diagnostic assistant, spotting patterns in complex data that a human might miss. This leads to faster, more accurate diagnoses and better treatment plans. AI handles the data, so clinicians can focus on care.
Whisperit is the voice‑first AI workspace built for legal and medical professionals, unifying dictation, drafting, and secure collaboration. Move from intake to export in fewer steps and reclaim your time. Learn more at https://whisperit.ai.