Healthcare Data Security: Your Complete Protection Guide
The Stark Reality Of Healthcare Security Threats
Healthcare data breaches are a constant and growing concern, affecting organizations of all sizes. These incidents aren't just news stories; they have real-world consequences for individuals and erode the public's trust in healthcare providers. Traditional security measures often fall short, unable to keep up with the rapid shift to digital systems and the ever-changing tactics of cybercriminals.
Why Healthcare Is a Prime Target
Several factors make the healthcare sector a prime target for cyberattacks. Protected health information (PHI) is highly valuable on the black market, fetching higher prices than credit card numbers or other personal data. This makes healthcare a lucrative target for financially driven attackers. The interconnected nature of healthcare systems, often relying on older technology and numerous third-party vendors like Epic, also creates multiple vulnerabilities. These weaknesses offer ample opportunities for unauthorized access.
The Expanding Threat Landscape
The methods used to breach healthcare data security are becoming increasingly sophisticated. While opportunistic attacks still occur, many cybercriminals now orchestrate complex, targeted campaigns designed to exploit vulnerabilities specific to medical environments. These attacks can range from ransomware, which disrupts operations by encrypting crucial data, to phishing campaigns designed to trick employees into divulging sensitive information.
Healthcare organizations must be ready to defend against a wider range of threats than ever before. The sheer scale of these attacks is also alarming. The frequency and magnitude of healthcare data breaches have risen dramatically in recent years. Between 2009 and 2024, 6,759 healthcare data breaches affecting 500 or more records were reported to the U.S. Office for Civil Rights (OCR). These breaches exposed the PHI of 846,962,011 individuals—over 2.6 times the U.S. population. In 2024 alone, an astounding 276,775,457 patient records were compromised, averaging 758,288 records per day. Find more detailed statistics here.
The Consequences of Inaction
Neglecting healthcare data security can have devastating repercussions. Beyond the financial costs of regulatory fines and remediation efforts, breaches can severely tarnish an organization's reputation and damage patient trust, leading to significant operational disruptions. This translates into real losses, including reduced patient numbers, difficulty attracting and retaining staff, and strained relationships with partners and stakeholders. The true cost of a breach goes far beyond the immediate incident.
Decoding Modern Cyber Attacks On Healthcare
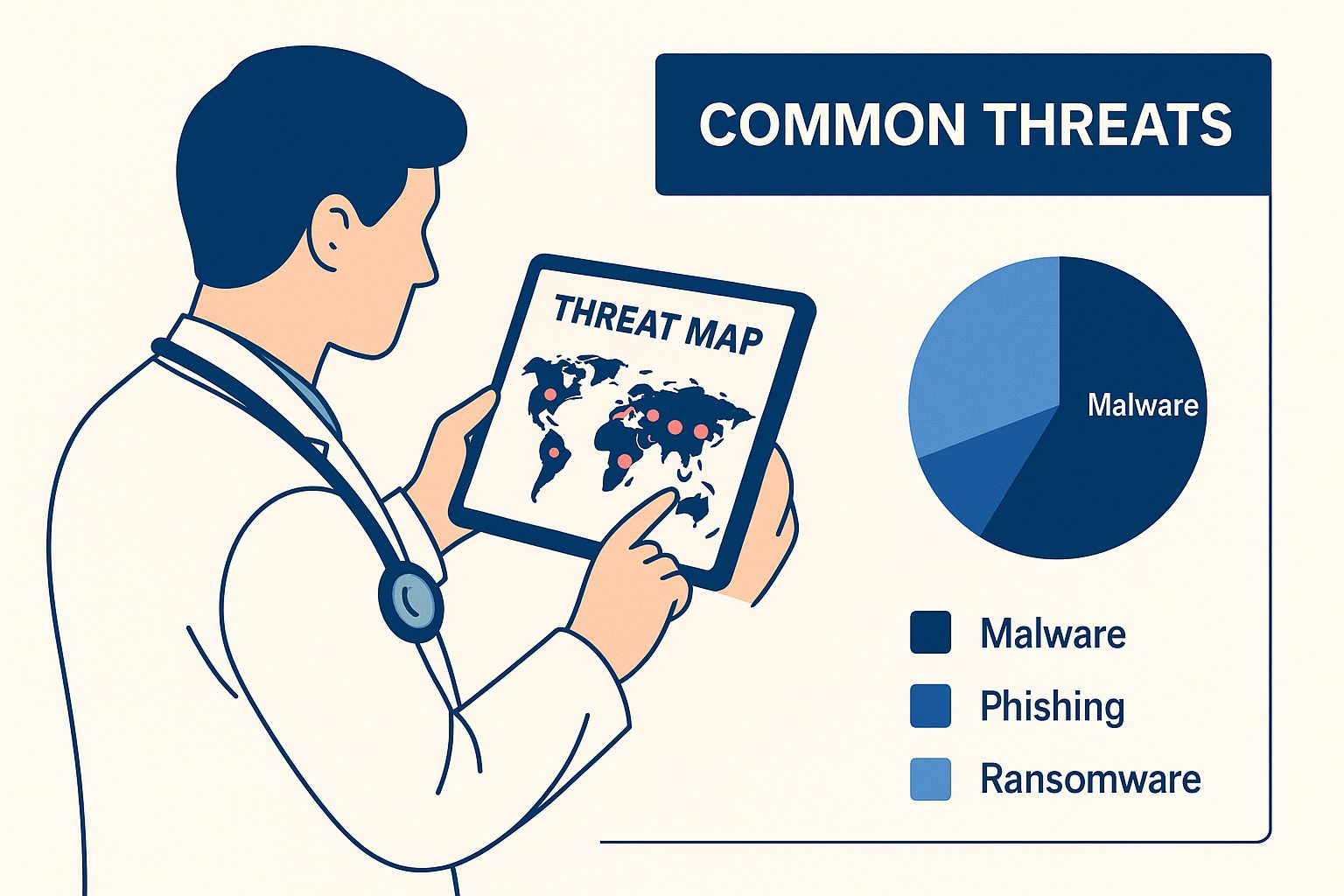
The infographic above shows a healthcare professional reviewing common digital threats on a tablet. This visual highlights the growing trend of attacks shifting from being opportunistic to employing more sophisticated methods. These attacks specifically target weak points within medical systems, taking advantage of their interconnectedness and the inherent value of patient data.
Beyond Malware: The Sophistication of Modern Threats
Cybersecurity threats have come a long way. Simple malware infections are now just a small part of a much bigger problem. Healthcare organizations today face complex, coordinated attacks designed to exploit the pressures of their daily operations.
Ransomware attacks, for example, are increasingly common, disabling critical systems and demanding large sums of money to restore access. Supply chain vulnerabilities also present a serious risk, as third-party vendors often have less stringent security measures, creating unexpected openings for attackers.
The Allure of Healthcare Data
Healthcare data is highly sought after on the dark web. It contains a treasure trove of personally identifiable information, including medical histories, financial details, and social security numbers. This makes it significantly more valuable than even credit card information.
As a result, healthcare is the third most targeted industry for cyberattacks. These attacks have evolved from opportunistic strikes to sophisticated, coordinated campaigns. These campaigns specifically target vulnerabilities within medical environments. You might be interested in this article: How to master reducing administrative costs in healthcare.
Adapting to Medical Environments
Attackers are constantly refining their methods to exploit healthcare settings. They understand the pressures faced by medical professionals and often exploit the urgency of patient care. Tactics can include impersonating medical staff to gain system access or launching phishing campaigns during busy periods.
Cybersecurity threats are the leading cause of healthcare data breaches. Since 2014, hacking and IT incidents have surpassed all other causes. They accounted for 80% of cases in 2022, a significant increase from just 4% in 2010. These incidents have affected 319 million individuals since 2009, a number approaching the entire U.S. population. For more on healthcare data breach statistics, see this article. Understanding how AI platforms handle sensitive information is vital. Data Security With Docsbot offers valuable insights into this aspect of modern healthcare security.
To understand how these threats have evolved over time, let's examine the following table:
Healthcare Cyber Threat Evolution by Year
| Year | Primary Threat Type | Percentage of Incidents | Records Affected (estimated) |
|---|---|---|---|
| 2010 | Insider Threats, Lost/Stolen Devices | 96% | Low (millions) |
| 2014 | Hacking, IT Incidents | ~50% | Medium (tens of millions) |
| 2018 | Ransomware, Malware | ~65% | High (hundreds of millions) |
| 2022 | Ransomware, Supply Chain Attacks | 80% | High (hundreds of millions) |
This table highlights the dramatic shift from traditional security issues like insider threats and lost devices to more digitally focused attacks. The increasing impact on records affected underlines the growing severity of these cyber threats.
Learning From the Front Lines
Security professionals with experience responding to real-world incidents emphasize a multi-layered approach to healthcare data security. This includes strong technical defenses and a robust security culture. This culture must be ingrained throughout the organization. Every team member needs to understand their role in safeguarding patient data. Healthcare organizations must make healthcare data security a top priority and constantly adapt their strategies to counter increasingly sophisticated attacks.
What A Healthcare Data Breach Really Costs You
The cost of a healthcare data breach goes far beyond the initial news stories and regulatory penalties. While these certainly capture attention, the true financial consequences are much more significant and long-lasting. A single breach can trigger a cascade of expenses, both immediate and long-term, potentially crippling an organization.
Immediate Costs: The First Wave of Damage
The first stage of a breach involves damage control, investigating the incident, and notifying affected parties. These immediate costs can include:
- Incident Response: Assembling a team of experts, often including external cybersecurity specialists, to manage the crisis.
- Forensic Investigation: Using detailed digital forensics to determine the root cause and the extent of the breach.
- Legal Counsel: Addressing complex regulatory requirements and potential lawsuits.
- Notification Costs: Communicating with affected patients and regulatory bodies, which can involve substantial administrative expenses.
- Credit Monitoring Services: Providing credit monitoring and identity theft protection services to those affected.
These upfront costs can quickly accumulate, placing a substantial burden on an organization’s financial resources. However, the financial repercussions do not end there.
Hidden Costs: The Long-Term Impact
The real cost of a healthcare data breach unfolds over time. These hidden costs can be even more damaging than the initial outlay:
- Reputational Damage: The loss of patient trust and negative media coverage can decrease patient volume and make it difficult to attract new patients. This damage can take years to repair.
- Operational Disruptions: Breaches can disrupt day-to-day operations, leading to canceled appointments, treatment delays, and a greater administrative workload.
- Staff Turnover: The stress and uncertainty in the aftermath of a breach can lead to staff burnout and higher turnover rates, further straining resources.
- Lost Revenue: Decreased patient volume, operational disruptions, and increased expenses all contribute to significant revenue loss.
- Increased Insurance Premiums: Cybersecurity insurance premiums are likely to increase following a breach, representing an ongoing expense.
Calculating Your Potential Exposure
Understanding the full financial ramifications of a data breach is critical for informed decision-making about security investments. Healthcare data is not only highly sensitive but is also set to become a dominant force in global data storage. Studies show that by the end of 2025, 36% of the world's stored data will be health-related. Alarmingly, 90% of this data remains inadequately protected. The resulting financial and operational impact is significant. In 2023, the average cost of a healthcare data breach reached $10.93 million per incident, encompassing regulatory fines and reputational damage. For more information, explore this article on Healthcare Data Security Trends.
Building a strong case for enhanced healthcare data security is essential. Articles like How to master data security and compliance can be helpful resources. By quantifying the potential cost of a breach, organizations can demonstrate the return on investment (ROI) of proactive security measures. This helps secure the funding needed to safeguard valuable data and maintain patient trust.
Building Healthcare Data Security That Actually Works

Generic security frameworks aren't sufficient for the intricate demands of healthcare. This sector requires specialized strategies that address the unique difficulties of safeguarding patient data while maintaining operational adaptability. Building robust healthcare data security necessitates a comprehensive strategy, encompassing everything from outdated legacy systems to the newest mobile technologies.
Risk Assessments Tailored to Healthcare
Effective healthcare data security begins with a comprehensive risk assessment. This assessment, however, needs to extend beyond typical IT practices and incorporate the realities of medical environments. For instance, consider the security ramifications of interconnected medical devices, the growing prevalence of mobile devices in clinical settings, and the dependence on third-party vendors. When establishing healthcare data security, robust security measures are paramount.
Policies That Protect Without Disrupting Care
Creating strong security policies is essential, but these policies must be meticulously designed to avoid obstructing crucial patient care. This requires close collaboration between security personnel and healthcare providers to achieve equilibrium between data protection and operational effectiveness. Policies should be clear, concise, and easily incorporated into current workflows.
Building a Strong Security Governance Structure
A well-defined governance structure is vital for accountability and oversight of healthcare data security initiatives. This includes establishing clear roles and responsibilities, implementing routine reporting procedures, and fostering a culture of security awareness organization-wide. Furthermore, security governance must remain flexible and adapt to the evolving requirements of the healthcare landscape. You may find this helpful: How to master security control frameworks.
Implementing Practical Strategies
Discussions with healthcare security leaders have revealed several practical strategies for building effective data security programs. These strategies include:
- Prioritizing risk-based approaches and concentrating resources on the most critical weaknesses.
- Implementing multi-factor authentication to strengthen access control.
- Conducting regular security awareness training for all staff.
- Developing incident response plans to address and mitigate potential breaches.
- Remaining informed about the latest security threats and best practices.
By adopting these measures, healthcare organizations can establish robust security that protects sensitive patient data without impacting the quality of care. This requires ongoing dedication and a commitment to continuous improvement. The New York Healthcare Cybersecurity Mandate underscores the growing importance of these measures, emphasizing multi-factor authentication and incident reporting. Its focus on Chief Information Security Officer roles highlights the critical need for dedicated leadership in this vital area.
Essential Tools For Healthcare Data Protection

Protecting patient data is paramount in healthcare. It requires more than just good intentions – it demands the right tools and a robust security posture. Choosing the right security solutions can be challenging, but prioritizing practical tools that integrate seamlessly with existing healthcare systems is crucial. This section explores essential security technologies, providing practical insights from professionals with real-world experience in medical settings.
Identity and Access Management (IAM)
Identity and Access Management (IAM) solutions form the bedrock of healthcare data security. IAM controls user access to sensitive information, employing methods like multi-factor authentication (MFA). MFA adds an extra layer of security by requiring multiple verification methods, such as a password combined with a unique code sent to a mobile device. This significantly hinders unauthorized access. Implementing strong identity verification and dynamic authorization are key to bolstering security. For more information on securing healthcare data, see our guide: How to master data security in healthcare.
Data Loss Prevention (DLP)
Data Loss Prevention (DLP) tools monitor and prevent sensitive data from leaving your organization's control. They identify and block attempts to send Protected Health Information (PHI) via email, cloud storage, or other methods. This is especially critical with the growing use of mobile devices and cloud-based systems in healthcare.
Intrusion Detection and Prevention Systems (IDPS)
Intrusion Detection and Prevention Systems (IDPS) actively monitor network traffic for malicious activity. These systems can identify and block known threats and detect unusual behavior that might signal an attack. This proactive approach is essential for swiftly identifying and mitigating security incidents before they escalate.
Encryption Software
Encryption scrambles data, rendering it unreadable without the correct decryption key. This safeguards information both in transit and at rest, protecting it even if a device is lost or stolen. Robust encryption is now a cornerstone of healthcare data security.
Security Information and Event Management (SIEM)
Security Information and Event Management (SIEM) tools collect and analyze security logs from across your organization’s systems. This allows security teams to identify patterns and anomalies that could indicate a breach. SIEM solutions provide a centralized view of security events, simplifying threat monitoring and response.
Endpoint Detection and Response (EDR)
Endpoint Detection and Response (EDR) solutions focus on securing individual devices like laptops, desktops, and mobile devices. EDR can monitor these endpoints for malicious activity, isolating infected systems, and preventing malware from spreading. Given the increasing use of mobile devices in healthcare, EDR is vital.
Comparing Essential Technologies
To help you understand the various options available, the following table compares these essential security technologies, outlining their strengths and weaknesses. It provides a clear comparison of protection levels, implementation difficulty, cost, and best use cases.
| Technology | Protection Level | Implementation Difficulty | Cost Range | Best Use Case |
|---|---|---|---|---|
| IAM | High | Moderate | Moderate to High | Controlling access to sensitive data |
| DLP | High | Moderate | Moderate | Preventing data exfiltration |
| IDPS | Moderate to High | Moderate to High | Moderate to High | Detecting and blocking network threats |
| Encryption | High | Moderate | Low to Moderate | Protecting data at rest and in transit |
| SIEM | High | High | High | Centralized security monitoring and analysis |
| EDR | Moderate to High | Moderate | Moderate | Securing individual devices |
This comparison can help healthcare organizations select the right security tools based on their unique needs and budget. The New York Healthcare Cybersecurity Mandate underscores the importance of many of these technologies, especially MFA. The mandate's requirements for incident reporting and the designation of Chief Information Security Officer roles highlight the need for a proactive and structured approach to healthcare data security.
Mastering HIPAA And Healthcare Security Regulations
Regulatory compliance, especially regarding HIPAA, can seem daunting. But instead of a burden, think of it as a strategic opportunity. A strong security program simplifies compliance and frees up resources.
HIPAA Compliance: A Practical Approach
HIPAA regulations might appear complex, but they center on core principles:
- Confidentiality: Shielding patient information from unauthorized access.
- Integrity: Maintaining data accuracy and preventing unauthorized changes.
- Availability: Ensuring reliable information access when needed.
These principles shape every facet of HIPAA compliance, from data storage and transfer to staff training and incident response. For further reading, explore How to master HIPAA compliant cloud storage.
Navigating Audits and Enforcement Actions
Understanding auditor expectations is vital for successful HIPAA compliance. Seasoned compliance officers recommend proactive steps like:
- Regular Risk Assessments: Pinpoint potential weaknesses and create mitigation plans.
- Comprehensive Documentation: Keep thorough records of policies, procedures, and training.
- Incident Response Plans: Develop clear protocols for handling security incidents and breaches.
These measures prepare organizations for audits and bolster their overall security. New York's Healthcare Cybersecurity Mandate, in effect from October 2, 2024, underscores this proactive approach. It emphasizes elements like multi-factor authentication and incident reporting. The mandate's focus on Chief Information Security Officer roles also highlights the increasing demand for dedicated security leadership.
Managing Business Associate Agreements
Business Associate Agreements (BAAs) are contracts that ensure third-party vendors handle Protected Health Information (PHI) securely. Effective BAA management requires:
- Due Diligence: Vetting vendors' security practices before signing an agreement.
- Ongoing Monitoring: Regularly checking vendors' HIPAA compliance.
- Clear Communication: Maintaining open communication channels to address security issues.
These practices protect your organization while fostering good vendor relationships.
Simplifying Compliance Through Robust Security
Strong security practices naturally support HIPAA compliance. By prioritizing data protection with measures like encryption, access controls, and staff training, organizations satisfy many HIPAA requirements. This proactive approach simplifies compliance and reduces administrative overhead. Investing in robust healthcare data security enhances an organization's reputation, builds patient trust, and contributes to improved care.
Creating A Healthcare Security Culture That Sticks
Technology plays a vital role in healthcare data security. However, robust systems alone aren't sufficient. Every individual within a healthcare organization, from doctors and nurses to administrative personnel, contributes to safeguarding patient information. This necessitates a security-conscious culture woven into the fabric of the organization. Let's explore practical strategies for cultivating this essential environment.
Building Awareness Through Engagement
Effective security awareness programs transcend mere checklists and mandatory training sessions. They actively engage healthcare professionals by connecting security practices to their daily responsibilities.
- Simulation Exercises: Realistic scenarios, such as simulated phishing attacks, empower staff to identify and respond to threats within a safe environment. This practical approach builds confidence and reinforces learned concepts.
- Peer Learning: Fostering teamwork and knowledge sharing establishes a supportive atmosphere for learning about security best practices. Peer-to-peer instruction can be a powerful tool, allowing team members to learn from each other's experiences and insights.
- Practical Scenarios: Anchoring security concepts to real-world situations within healthcare settings amplifies the training's impact. When staff understand the direct relevance of security protocols to their daily work, they are more likely to embrace them.
These interactive methods encourage active participation, transforming security training from a chore into a valuable professional development opportunity.
Integrating Security Into Clinical Workflows
Security training should be seamlessly woven into existing clinical workflows. This can be achieved through bite-sized microlearning modules, short informative videos, and interactive quizzes incorporated into current training platforms or professional development activities. This approach minimizes disruption to busy schedules while reinforcing essential security principles.
Many successful organizations embed security reminders directly within Electronic Health Record (EHR) systems. For instance, prompts can appear before accessing sensitive patient data, reminding staff of appropriate procedures. This consistent reinforcement helps integrate security practices into daily routines.
Measuring and Maintaining Engagement
Evaluating the effectiveness of security awareness initiatives is paramount. Several methods can be employed to track progress and identify areas for improvement.
- Regular Assessments: Periodic quizzes and practical exercises help gauge staff comprehension of security protocols. These assessments provide valuable data on knowledge retention and identify any gaps in understanding.
- Feedback Mechanisms: Surveys and anonymous feedback channels offer crucial insights into the program's efficacy and highlight areas for enhancement. Gathering feedback directly from staff helps tailor the program to their specific needs and concerns.
- Performance Tracking: Monitoring security-related incidents, such as reported phishing attempts or accidental data disclosures, provides quantifiable data on behavioral change. This data-driven approach allows organizations to measure the tangible impact of their security awareness efforts.
Sustaining engagement requires continuous effort. Regular updates, refresher training, and recognition programs keep security top-of-mind. Building a healthcare data security culture is an ongoing journey, not a one-time project. Investing in a human-centered approach empowers organizations to ensure their security measures yield tangible improvements and lasting protection for sensitive patient data.
Ready to bolster your organization's security posture and safeguard sensitive information? Discover how Whisperit’s AI-powered platform can optimize your documentation workflows while prioritizing data privacy and security.