A Guide to Healthcare Compliance Software
Healthcare compliance software is a specialized system built to help medical organizations manage, track, and automate their adherence to the maze of government and industry regulations. Think of it as a central command center for everything related to compliance, from managing internal policies and employee training to handling incident reports.
Navigating Healthcare Regulations with Confidence
Trying to manage healthcare compliance without the right tools can feel like navigating a stormy sea in a rowboat—no map, no compass, just constant, unpredictable waves. The currents of regulatory change are always shifting, and the waters are full of serious risks, from massive fines to crippling data breaches. Reaching the safe harbor of complete, auditable compliance can feel next to impossible.
This is where healthcare compliance software becomes your essential navigation system. It’s specifically designed to bring clarity and control to this incredibly complex environment. Instead of seeing compliance as just another frustrating cost, this technology helps you reframe it as what it truly is: the bedrock of patient trust and operational integrity.
The Core Problems It Solves
At its core, this software tackles the overwhelming administrative burden and the high-stakes nature of healthcare rules. It creates a structured framework for handling key regulatory mandates and solves several critical problems that plague healthcare providers.
- Automates Manual Work: It gets rid of error-prone spreadsheets and paper checklists. Instead, it uses automated workflows to track policy updates, training completions, and incident investigations, saving time and reducing human error.
- Centralizes All Documentation: Every compliance-related document, from internal policies to formal audit reports, is stored in one secure, easily accessible place. Our essential guide to healthcare documentation standards explains in more detail why this is so critical.
- Provides Real-Time Visibility: Dashboards give compliance officers an instant, live look at the organization's standing, flagging potential risks long before they can escalate into costly violations.
- Simplifies Audits: The software automatically creates a clear, chronological audit trail. When regulators come knocking, proving due diligence is straightforward.
In essence, healthcare compliance software moves an organization from a reactive, chaotic state to a proactive, controlled one. It transforms compliance from a source of anxiety into a manageable and measurable business process.
The demand for these tools is skyrocketing for a reason. The global market, valued at USD 1.8 billion in 2023, is expected to surge to over USD 5.2 billion by 2032. This explosive growth is fueled by the severe financial penalties tied to non-compliance with regulations like HIPAA and GDPR.
Of course, software is a powerful tool, but it's just one piece of a comprehensive strategy. For complex situations, many organizations find that partnering with a source of specialized compliance legal advice offers an essential layer of protection. This guide will walk you through how to pair the right technology with smart processes to build lasting confidence in your compliance program.
The High Cost of Manual Compliance Methods

Relying on spreadsheets and paper checklists to manage healthcare compliance is like trying to navigate a modern highway with a paper map from 1985. It might feel familiar, but it’s dangerously out of date and unprepared for the complexities you'll actually face. A simple human error, like a misplaced file or a forgotten signature, can easily escalate into a full-blown compliance disaster.
The consequences of these manual oversights aren't just a possibility; they're a painful reality for many organizations, often measured in seven-figure fines and damaged reputations. A single slip-up in handling protected health information (PHI) can trigger a government audit, bringing penalties that could cripple a healthcare practice. Even without a breach, the operational drag is immense, with staff sinking countless hours into just chasing down paperwork.
Moving from manual methods to a dedicated software solution is no longer just a good idea—it's a financial necessity. The stakes are simply too high to ignore. For example, Aetna paid nearly one million USD in a 2020 HIPAA settlement for failing to uphold basic privacy standards. When you consider that healthcare data breaches cost the industry an estimated $6.45 million annually, the argument for adopting healthcare compliance software makes itself. You can dig deeper into these numbers by exploring the market data on Grand View Research.
The Limits of Spreadsheets and Binders
At their core, manual systems just can't provide the real-time oversight and scalability that modern healthcare demands. A compliance program built on Excel files and three-ring binders is inherently fragile and opaque. It’s riddled with weaknesses that dedicated software is specifically designed to fix.
These old-school systems crumble under the weight of constant regulatory changes. A minor update to a HIPAA rule can set off a chain reaction, demanding dozens of policy tweaks, new training sessions, and verified sign-offs from every single employee. Trying to track that process by hand is a recipe for failure.
A spreadsheet won't ping you when a Business Associate Agreement is about to expire. A paper checklist can't prove that an employee actually completed their security training on a specific date. These static tools create a false sense of security while dangerous compliance gaps hide just beneath the surface.
The True Operational Burden
Beyond the risk of massive fines, the day-to-day operational drain of manual compliance is staggering. Just think about the workflow for a simple policy update.
- Drafting and Approval: The new policy starts as a Word document, which gets emailed back and forth between managers. This quickly creates a confusing mess of different versions.
- Distribution: Once finalized, the policy is blasted out via email, but there's no good way to track who has actually read and understood it.
- Verification and Storage: Managers are left to manually chase down signatures. Those signed papers then get shoved into a filing cabinet, where they're a headache to find during an audit.
This entire process is slow, inefficient, and creates opportunities for error at every turn. It pulls skilled staff away from what they should be doing: focusing on patient care and other high-value work. To see just how many moving parts there are, have a look at our guide on the HIPAA compliance requirements checklist. You'll quickly see why automating these tasks isn't just about avoiding risk—it's about getting valuable time and focus back.
Connecting Regulations to Software Features
Trying to make sense of dense legal jargon in regulations like HIPAA, HITECH, and OSHA can feel like a losing battle. The language is complex, but what does it actually demand from your daily operations? The trick is to translate these abstract rules into practical, everyday actions—and this is precisely where healthcare compliance software shines.
This software essentially builds a bridge, directly connecting what the law says you must do with specific tools that help you get it done. Instead of just reading about the HIPAA Security Rule, you can implement its requirements using software functions like automated access controls and continuous audit trails. It turns dense legalese into a concrete, manageable checklist.
This infographic shows how major regulations like HIPAA, GDPR, and ISO 27001 are addressed by core compliance software modules.
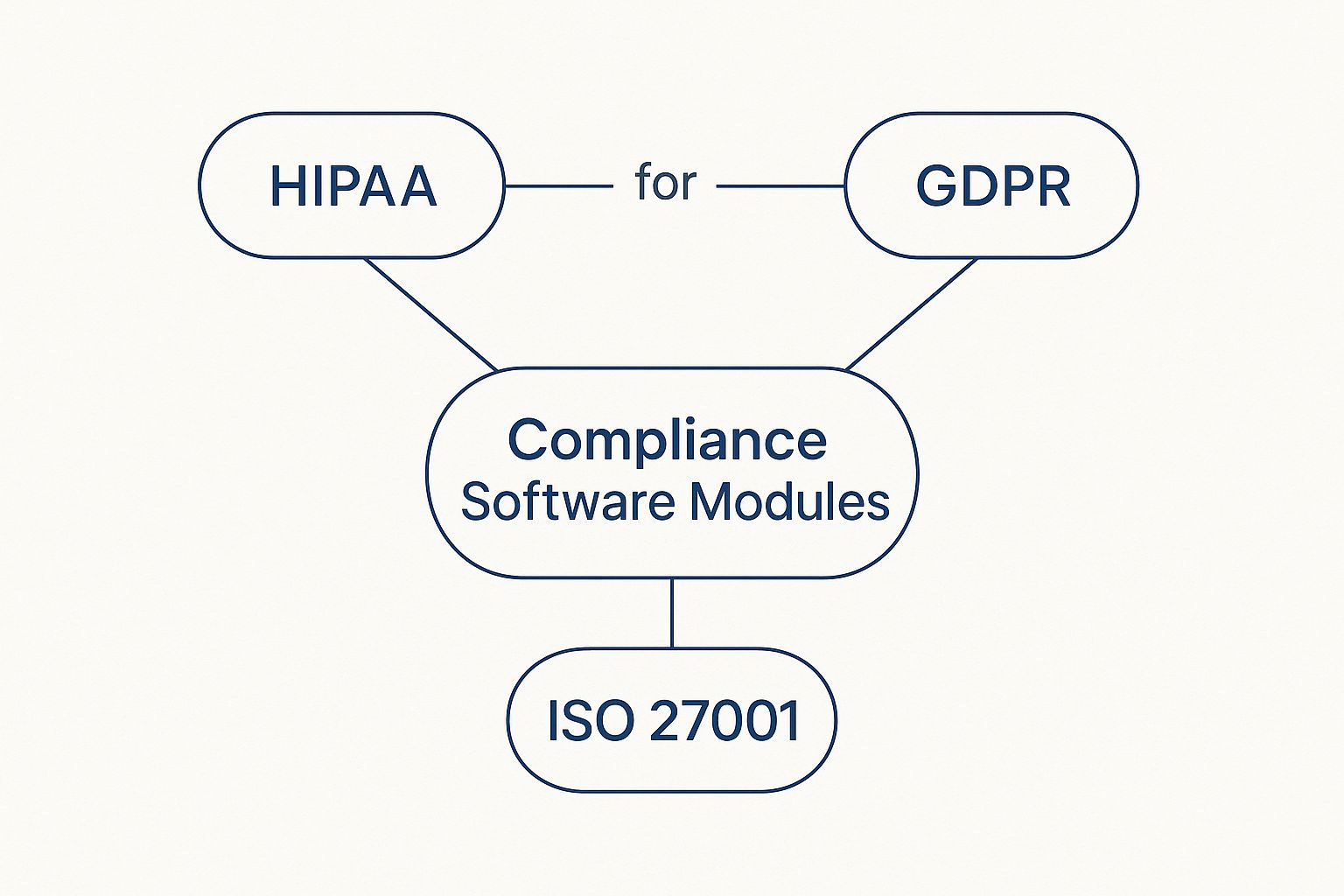
The image makes it clear: while each regulation has its own focus, their core requirements often overlap. A unified software platform can manage these interconnected demands from a single command center.
From HIPAA Rules to Software Solutions
The Health Insurance Portability and Accountability Act (HIPAA) is the foundation of patient privacy in the U.S. It isn't a single, monolithic rule, but rather a collection of components, each with demands that are perfectly suited for software automation.
- The Privacy Rule: This part governs how Protected Health Information (PHI) is used and shared. Software helps manage this by digitizing patient consent forms, tracking disclosures, and enforcing role-based access to ensure PHI is only seen on a need-to-know basis.
- The Security Rule: Here, the focus is on protecting electronic PHI (ePHI). A solid compliance platform handles this with features like data encryption, multi-factor authentication, and tools for running regular security risk assessments to find and fix vulnerabilities before they become a problem.
- The Breach Notification Rule: If a breach happens, you have to follow strict notification procedures. An incident management module acts as your guide, walking you through every step—from discovery and investigation to notifying affected individuals and HHS—to make sure you hit every deadline.
This intense focus on regulation is a big reason why North America dominates the healthcare compliance software market. The United States, in particular, drives this trend, accounting for roughly 52% of global revenue. Its market segment is estimated at a staggering USD 1.22 billion in 2024, fueled by strict HIPAA enforcement and the widespread adoption of digital health tools. For a deeper analysis, you can explore the full market research on GII.
HITECH and OSHA: The Supporting Pillars
While HIPAA often steals the spotlight, other regulations add critical layers that software helps manage.
The HITECH Act gave HIPAA more teeth by increasing penalties for non-compliance and promoting the use of secure electronic health records. Software addresses HITECH by providing auditable proof of your compliance activities, which is your best defense during an investigation. Similarly, OSHA (Occupational Safety and Health Administration) requires a safe workplace, covering everything from bloodborne pathogen training to tracking on-the-job incidents.
A good compliance platform with built-in training modules can assign and track both annual HIPAA refreshers and OSHA-mandated safety courses. This shows how a single system can help you stay on top of multiple, distinct regulations at once. To learn more about how all these pieces fit together, check out our ultimate guide on compliance management solutions.
Mapping Regulations to Essential Software Features
To make this connection crystal clear, this table breaks down how key healthcare regulations are met by specific software features. Think of it as a map from the problem (the regulation) to the solution (the software tool).
Mapping Regulations to Essential Software Features
| Regulation | Core Requirement | Essential Software Feature |
|---|---|---|
| HIPAA Security Rule | Conduct regular risk analyses to identify threats to ePHI. | Automated Risk Assessment Module: Guides users through assessments, pinpoints vulnerabilities, and tracks remediation tasks. |
| HIPAA Privacy Rule | Ensure PHI is only accessed by authorized individuals. | Role-Based Access Controls: Restricts data access based on job function, enforcing the "minimum necessary" standard. |
| HITECH Act | Maintain verifiable proof of all compliance activities. | Centralized Audit Trails: Logs every user action, creating an unchangeable record of who accessed what data, and when. |
| Breach Notification Rule | Report data breaches to authorities and individuals promptly. | Incident Management & Reporting: Provides checklists and timers to guide breach response according to strict legal deadlines. |
| OSHA Standards | Train employees on workplace safety and health hazards. | Learning Management System (LMS): Assigns, delivers, and tracks completion of required safety training courses and certifications. |
As you can see, healthcare compliance software is far more than an administrative tool; it's a strategic asset for managing risk. It directly translates dense legal requirements into functional, automated processes that protect both your patients and your organization.
Core Features of Modern Compliance Platforms

So, you understand the why behind healthcare compliance software. Now comes the tricky part: knowing what features actually matter. The truth is, not all platforms are built the same. The best ones aren't just digital filing cabinets for policies; they are active, intelligent systems with specific tools designed to tackle the biggest compliance headaches head-on.
Think of it like a master mechanic’s toolbox. You don't just have a pile of tools; you have trays organized for specific jobs—wrenches here, diagnostic computers there. Good compliance software works the same way, organizing its features to solve distinct problems. Let's pop the hood and look at the essential tools every organization should expect to find.
Tools for Proactive Risk Management
The old way of doing compliance was reactive. You waited for a problem and then fixed it. Modern compliance is all about getting ahead of the curve. This is where risk management features shine, helping you spot and patch up weak points before they ever turn into a costly breach or a hefty penalty.
- Automated Risk Assessments: Forget wrestling with manual checklists and spreadsheets. The software walks you through structured security and privacy assessments based on frameworks like HIPAA. It automatically flags potential issues, assigns a risk score, and helps you build a clear, prioritized action plan. This turns a dreaded annual task into a continuous, manageable process.
- Risk Heat Maps: These are brilliant. A risk heat map gives you a simple, color-coded visual of your organization's entire risk landscape. High-risk areas might glow red, moderate risks yellow, and low risks green. In a single glance, a compliance officer knows exactly where to focus their attention and resources.
These features take the guesswork out of risk management, turning it into a data-driven strategy. You gain the foresight to see where your defenses are thin and the tools to shore them up.
Functions for Streamlined Audit Management
Audits are a fact of life in healthcare, but they don't have to be a code-red panic. The right healthcare compliance software makes audit prep a part of your daily routine, not a frantic, last-minute scramble. The goal is to be "audit-ready" all the time.
The term "audit trail" often sounds technical, but it’s simply the digital proof that shows who did what, and when. It’s the irrefutable evidence that turns a stressful, accusatory audit into a simple exercise of pulling a report.
The best audit management features provide this proof on demand.
- Centralized Audit Trail Logging: Every single action taken in the platform—from a policy being updated to a file being accessed—is automatically logged with a user ID and a timestamp. This creates an unchangeable record that serves as your single source of truth when a regulator comes knocking.
- Customizable Audit Checklists: Most platforms come pre-loaded with checklists for major audits (like HIPAA or OSHA), but they also let you create your own for internal reviews. This ensures everyone follows the same script, whether you're facing a government inquiry or just doing a routine internal check.
- Incident Management and Reporting: When a potential breach happens, this module is your command center. It guides your team through the necessary investigation, documentation, and reporting steps, often with built-in timers to make sure you meet the strict notification deadlines required by the Breach Notification Rule.
Capabilities for Robust Policy Management
Policies are the foundation of your entire compliance program. But they’re completely useless if they’re outdated, buried on a shared drive, or ignored by staff. Policy management tools make sure your rules are living, breathing documents that actually guide how people work.
The Lifecycle of a Policy
- Creation and Collaboration: Draft policies right inside the platform. Stakeholders can comment and approve changes in one place, which means no more digging through endless email chains to find the latest version.
- Distribution and Attestation: Once a policy is approved, it's automatically pushed out to the right employees. The system then tracks who has opened it, read it, and electronically signed off, creating a bulletproof record that they understand the rules.
- Ongoing Maintenance: The software sends automated reminders when it's time for a policy's annual or biennial review. This simple feature ensures your critical documents never become stale.
This automated lifecycle takes one of the most tedious administrative burdens off your plate. It guarantees your policies are always current, effectively distributed, and demonstrably understood by your staff, which is how you build a true culture of compliance from the ground up.
How to Choose the Right Compliance Software

Choosing the right healthcare compliance software is a huge decision. It's not just about ticking a box; you're investing in a system that will become the bedrock of your risk management strategy, protecting your patients, your staff, and your practice’s reputation. If you rush this or pick a one-size-fits-all solution, you could easily end up with more headaches than you started with.
The best approach is to be methodical. Think of it like a doctor performing a diagnosis. You wouldn't prescribe a treatment plan without a complete patient history and a thorough examination. In the same way, you shouldn't even start looking at software until you've done a deep dive into your own practice to understand exactly what hurts.
Start With an Internal Needs Assessment
Before you open a single vendor website, you have to look inward. A successful software rollout always begins with a crystal-clear picture of what you need to fix. Get your key people in a room—your compliance officer, IT lead, a head clinician, and an administrator—and start asking some tough questions.
- What are our biggest compliance struggles right now? Is it keeping track of employee training, managing mountains of BAAs, or just getting risk assessments done on time?
- Where are our manual processes causing friction or creating risk? Get specific. Pinpoint the workflows that are slow, prone to human error, or a nightmare to audit.
- Which regulations keep our team up at night? Are we constantly worried about specific HIPAA Security Rule mandates or tripping over OSHA reporting deadlines?
The answers to these questions become your shopping list of core requirements. This list is your North Star. It will guide every decision you make and stop you from being swayed by flashy features that don't actually solve your day-to-day problems. Focusing on what truly improves your operations is a cornerstone of a well-run practice, and our guide on healthcare process improvement has more ideas on how to sharpen your workflows.
Key Criteria for Evaluating Software Vendors
Once you know exactly what you need, you can begin the hunt for the right software partner. Your goal is to find a solution that not only solves today's problems but can also adapt as your organization grows and changes.
A great software platform should feel like a partner in compliance, not just a tool. The vendor's expertise, support, and vision are just as important as the features in their software.
Look past the glossy brochures and sales pitches. You need to scrutinize any potential vendor on these make-or-break factors:
- Scalability: Can the software grow with you? A tool that’s perfect for a 10-person clinic needs to be able to expand to serve a 100-person medical group without forcing you to start from scratch.
- Integration Capabilities: How well does it play with others? Specifically, you need to know how it connects with your Electronic Health Record (EHR). Seamless integration is non-negotiable for preventing data chaos and maintaining a single source of truth.
- Vendor Support and Training: What happens after you sign the contract? Find out what their onboarding looks like. Do they provide ongoing support and user-friendly training? A powerful tool is worthless if your team finds it too confusing to use.
- Transparent Pricing: Demand clear, straightforward pricing. No one likes surprise fees. Make sure you understand exactly what you're paying for—from the number of users to access to different features.
The Vendor Demo Litmus Test
The live demo is where the rubber meets the road. This is your chance to put both the software and the vendor through their paces. Don't sit back and watch a generic, canned presentation. Arrive with a list of specific questions drawn directly from your internal assessment.
To help you stay organized and compare your options fairly, use a simple checklist. This ensures you're evaluating every vendor on the same critical points.
Software Evaluation Checklist
| Evaluation Criteria | Vendor A | Vendor B | Notes |
|---|---|---|---|
| Meets Core Needs | ☐ Yes ☐ No | ☐ Yes ☐ No | Does it solve our top 3 compliance problems? |
| EHR Integration | ☐ Native ☐ API ☐ None | ☐ Native ☐ API ☐ None | How complex is the integration process? |
| User-Friendly Interface | ☐ Yes ☐ No | ☐ Yes ☐ No | Is the dashboard intuitive for non-technical users? |
| Training & Support | ☐ Included ☐ Add-on | ☐ Included ☐ Add-on | What is the typical support response time? |
| Pricing Transparency | ☐ Clear ☐ Vague | ☐ Clear ☐ Vague | Are there extra costs for more users or data? |
During the demo, ask them to show you exactly how their system handles one of your real-world pain points. For instance: "Show me the exact workflow for onboarding a new nurse, assigning them required HIPAA training, and tracking their policy signature."
How they handle that direct request will tell you far more about their product and their company than any polished slide deck ever could.
Your Top Compliance Software Questions, Answered
Even after you've weighed the features and benefits, it's natural to have a few more questions before committing to a new system. Making the right choice means getting straight answers to those practical "what if" and "how does this actually work" queries that pop up. This section is all about addressing the most common questions we hear about healthcare compliance software.
Think of this as a final Q&A session to clear up any lingering doubts. My goal is to give you the confidence that you have all the information you need to move forward.
How Does This Software Help With Staff Training?
One of the biggest wins with modern compliance software is how it handles the entire training process from start to finish. You can assign specific courses—like the annual HIPAA security awareness training—to different roles or departments. The system then takes over, automatically nudging employees who are behind schedule and tracking who has completed what, all in real-time.
This gives you a rock-solid, auditable trail that proves your team has been trained on essential policies. It completely does away with the old, error-prone method of managing training with spreadsheets. Instead, you get a single dashboard to see your organization’s progress and spot any knowledge gaps instantly.
Is Compliance Software Useful For A Small Practice?
Absolutely. In fact, you could argue it's even more crucial for smaller practices. A solo practitioner or small clinic has to meet the same demanding regulations—and faces the same crushing fines—as a major hospital network, but they're doing it with a fraction of the resources. Many software providers now offer scalable, cloud-based tools with pricing that makes sense for smaller organizations.
The real game-changer for a small practice is automation. The software handles the monotonous but critical admin work like risk assessments, policy updates, and training records. These are the tasks that would otherwise steal valuable time from a clinician or an office manager. It’s about getting enterprise-level compliance protection at a price you can afford, dramatically lowering your risk, no matter your size.
What Is The Difference Between EHR Features and Dedicated Compliance Software?
This is a great question, and the confusion is common. An Electronic Health Record (EHR) is built to protect the patient data inside it. Think of its security features, like user access controls and audit logs, as a vault for the data itself.
Dedicated healthcare compliance software, however, manages your organization's entire compliance program. Its scope is much wider. It’s responsible for things like:
- Managing all policies and procedures across every department.
- Conducting organization-wide security and privacy risk assessments.
- Handling incident reporting and the entire investigation workflow.
- Tracking Business Associate Agreements (BAAs) and other vendor contracts.
- Overseeing employee training on topics that go far beyond the EHR, like OSHA safety protocols.
Simply put, your EHR secures the data, while compliance software makes sure the people, policies, and processes surrounding that data are airtight. Since strong policies are the bedrock of any program, it's worth brushing up on document management best practices to see how everything fits together.
How Long Does Implementation Usually Take?
The timeline really depends on the size and complexity of your organization. For a small practice going with a standard cloud-based platform, you could be up and running in just a few weeks. But for a large hospital system with multiple locations and a ton of historical data to import, the process could take several months to fully complete.
Any good vendor will give you a clear, step-by-step implementation plan right from the get-go. This should always include hands-on help with migrating your data and thorough training for your team to make the switch as painless as possible. For more ongoing discussions about navigating new rules, you can also Discover additional insights on healthcare compliance from other experts in the field.
Ready to cut down on manual documentation and ensure your practice remains secure and compliant? Whisperit offers advanced AI dictation and transcription with a focus on Swiss-hosted security and privacy. See how professionals are completing paperwork twice as fast by visiting https://whisperit.ai.