Electronic Health Record Optimization Tips to Improve Care
Optimizing your electronic health record system isn't about piling on more bells and whistles. It's about strategically clearing the path so clinicians can focus on what matters: patient care. A successful overhaul is built on a solid plan—one grounded in real-world workflows, insights from your whole team, and goals you can actually measure.
Building Your Foundation for EHR Optimization
Jumping straight into software settings without a clear strategy is a surefire way to waste time and resources. True EHR optimization begins long before you touch a single configuration file. It starts with a deep, honest look at your organization's unique pain points and what you truly want to achieve. The whole point is to move beyond fuzzy ideas like "improving efficiency" and make tangible, impactful changes.
Think of this first stage as diagnosis before prescription. It involves getting a clear picture of how your teams actually work, not just how the system was designed to be used. Too many optimization projects fail because they're driven solely by IT, completely ignoring the invaluable, on-the-ground knowledge of frontline staff.
Conduct a Thorough Workflow Analysis
First things first: you need to map out your current clinical and administrative workflows. This is more than just drawing up process diagrams. It means shadowing real users—physicians, nurses, MAs, and administrative staff—to see firsthand where the system is getting in their way.
Keep an eye out for these common frustrations:
- Repetitive Data Entry: Where are staff typing the same information into multiple fields or screens?
- Excessive Clicks: Which routine tasks require a frustrating number of clicks to navigate through endless menus?
- Creative Workarounds: What unofficial shortcuts or "hacks" have users invented to get around system limitations? These are goldmines for identifying core problems.
- Information Overload: Are your users drowning in irrelevant alerts or data fields that just slow them down?
Discovering that a nurse spends five minutes per patient navigating three different screens just to document vitals is a concrete problem you can actually solve. This is the kind of granular insight that makes a real difference.
Assemble a Cross-Functional Team
An EHR touches every single part of your organization, and your optimization team needs to reflect that. A project led only by IT specialists or administrators will almost certainly miss the practical realities of day-to-day patient care.
Your team should absolutely include:
- Physician Champions: Respected clinicians who can advocate for changes and provide a doctor's perspective on what works and what doesn't.
- Nursing Representatives: Nurses often spend the most hands-on time with the EHR. They are your best source for pinpointing workflow bottlenecks.
- Administrative Staff: Your front desk and billing folks can highlight issues with patient registration, scheduling, and the revenue cycle.
- IT and Informatics Specialists: These are the technical experts who know the system's capabilities and limitations inside and out.
This kind of collaborative approach ensures that any solutions are both technically sound and clinically practical, which dramatically increases the odds of successful adoption. Meaningful training is also a huge piece of the puzzle. For more on that, check out our guide on effective electronic health records training for strategies that actually stick.
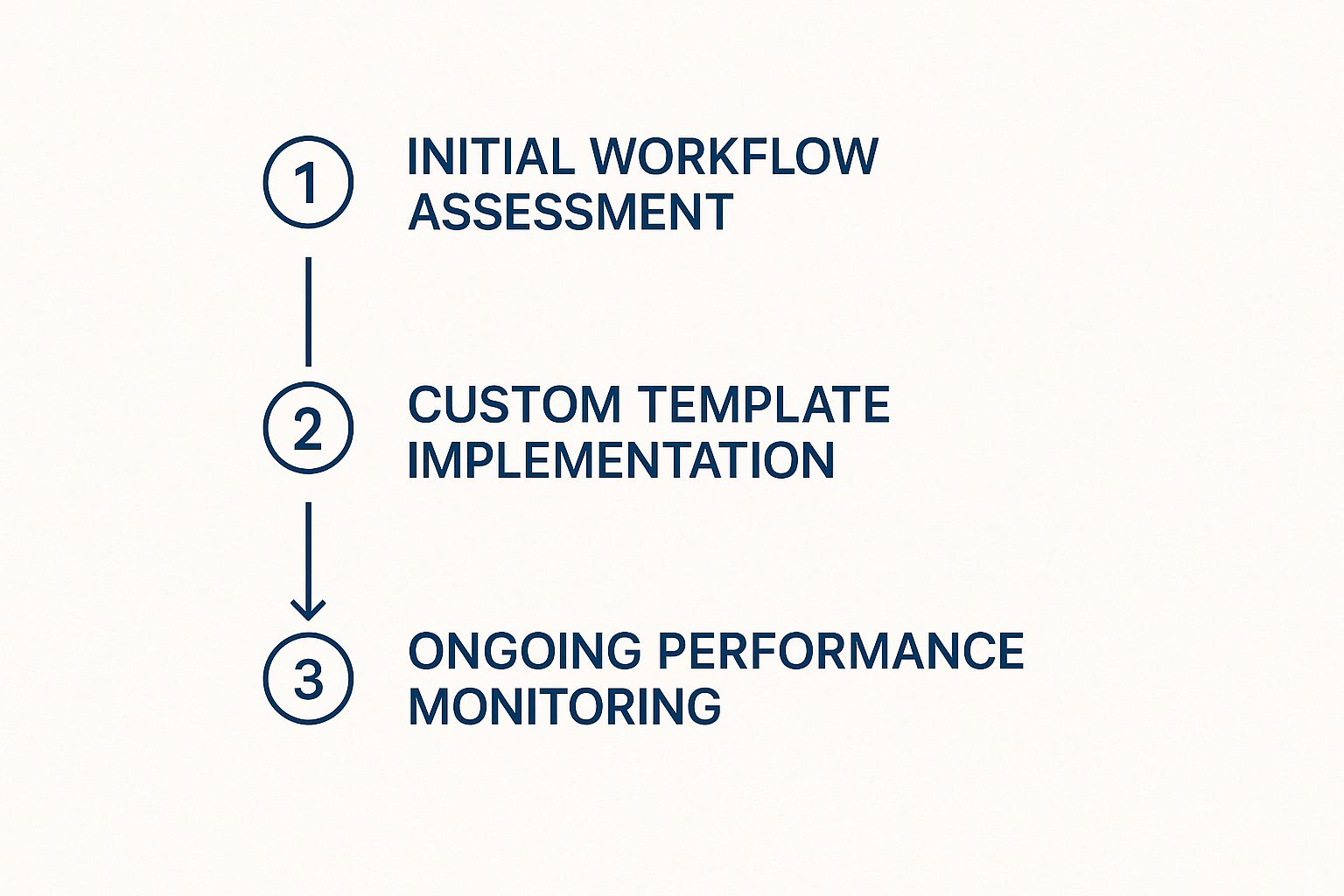
This process flow shows that optimization isn't a one-and-done project. It's a continuous cycle of evaluation, refinement, and improvement.
Define Specific and Measurable Goals
Vague objectives always lead to vague results. Instead of a fuzzy goal like "enhance user satisfaction," you need to set specific, quantifiable targets that directly address the bottlenecks you’ve uncovered.
The most effective EHR optimization initiatives are driven by data, not assumptions. By setting clear KPIs from the start, you create a framework for measuring success and demonstrating tangible ROI to stakeholders.
For example, you can transform your goals into measurable outcomes like these:
- Reduce Documentation Time: Decrease the average time to complete a standard patient note by 25% within three months.
- Minimize Order Errors: Lower medication order entry errors by 15% in the next quarter.
- Improve System Usability: Increase the clinician satisfaction score on the EHR usability survey from 65 to 80.
These efforts are critical. The drive for better healthcare IT is global, and EHR adoption rates show just how widespread these systems have become. In the United States, for instance, over 95% of hospitals have implemented EHR systems. In many European countries, the numbers are even higher—the Netherlands and the UK see 99% of primary care physicians using EHRs, with Sweden (98%) and Australia (97%) close behind.
By establishing this solid foundation—built on clear analysis, a diverse team, and measurable goals—your EHR optimization project is set up for success right from the start.
Designing a User-Centric Clinical Workflow
Let's be honest: an EHR is only as good as the experience of the person using it. If your clinicians find the system clunky, confusing, or slow, even the most powerful features are worthless. True electronic health record optimization is all about putting the user—the physician, nurse, or MA—at the absolute center of the design.
This means we have to stop thinking about technical specs and start focusing on the real human interactions that happen dozens of times a day. The goal is to make the software feel invisible, letting providers concentrate on their patients instead of their screens.

Customize Templates and Order Sets for Specialties
One of the fastest ways to win back time is by tailoring the EHR to specific clinical specialties. A generic, one-size-fits-all setup is a recipe for frustration. It forces users to wade through irrelevant fields and click endlessly, adding friction to every single patient encounter.
Think about a busy orthopedic surgeon trying to document a knee replacement follow-up. Why should they have to scroll past pediatric vaccination schedules or obstetric history fields? It’s more than just an annoyance; it’s a major time sink that contributes directly to burnout.
The answer is building out specialty-specific templates.
- For Cardiology: A new patient template could pre-populate fields for chest pain characteristics, cardiac risk factors, and relevant family history.
- For Pediatrics: Design well-child visit templates organized by age, with built-in prompts for developmental milestones and required immunizations.
- For Dermatology: Develop templates with body maps for pinpointing lesion locations and pre-filled procedural notes for common biopsies.
In the same way, customized order sets can slash the number of clicks needed. Instead of hunting for individual labs, imaging, and meds for something like community-acquired pneumonia, a physician can select one order set that bundles all the usual suspects, then tweak it as needed.
Declutter the User Interface
Visual clutter is the enemy of efficiency. When a screen is jammed with dozens of fields, buttons, and alerts, it overwhelms the user and makes it hard to find what actually matters. A huge part of optimizing an EHR is simply getting rid of the noise.
Work with your IT or informatics team to hide or disable fields that certain roles never use. A medical assistant, for example, probably doesn't need to see complex billing codes. A primary care doc might not need access to surgical scheduling modules.
A cleaner, more focused interface doesn't just look better—it functions better. By removing unnecessary elements, you guide the user's attention to the most critical tasks, reducing errors and saving precious seconds on every single interaction.
Another powerful way to reduce friction is implementing single sign-on (SSO). Juggling separate logins for the EHR, lab portal, and imaging system creates password fatigue and wastes time. SSO gives clinicians one secure, seamless entry point to all the platforms they need.
Implement Practical, Time-Saving Features
Sometimes, the smallest tweaks have the biggest impact. Something as simple as creating a "smart phrase" or macro for a routine follow-up note can save a physician several minutes per patient. Over a busy week, that adds up to hours of reclaimed time.
To get you started, here’s a quick look at some proven, high-impact optimizations.
| High-Impact Workflow Optimization Techniques | | :--- | :--- | :--- | | Optimization Tactic | Primary Benefit | Impacted Roles | | Pre-populated Notes | Reduces documentation time for common, stable conditions. | Physicians, Nurse Practitioners | | Role-Based Dashboards | Displays only relevant information and tasks for each user. | All Clinical & Admin Staff | | Integrated Communication | Allows secure messaging within the EHR, replacing external apps. | All Clinical Staff | | Favorite Lists | Creates shortcuts for frequently ordered medications or diagnoses. | Prescribing Clinicians |
These practical changes show that you're listening to your team's needs.
Ultimately, this human-centered approach is what separates a frustrating EHR from a helpful one. The real challenge isn't just adding new features; it's making them intuitive and genuinely useful in the chaotic reality of a clinic.
To make documentation even faster, it’s worth exploring affordable dictation software alternatives, especially those built for medical use. This helps reduce dependence on manual typing. As you get these workflows humming, you can push things even further; learn more about workflow automation in healthcare to see how to take your efficiency to the next level.
Ensuring Data Integrity and Interoperability
An optimized EHR is so much more than a fast, slick interface. It runs on data. If that data isn't clean, reliable, and easily shareable, the whole system's value collapses. That’s why a rock-solid data foundation, built on consistency and trust, is the real secret to true electronic health record optimization.
This trust is what lets clinicians make critical decisions with confidence. Without it, the EHR just becomes another administrative headache instead of a powerful clinical tool. The real aim here is to make sure every piece of information is accurate, structured, and available exactly when and where it's needed.
Standardize Data Entry Protocols
The biggest enemy of data integrity? Inconsistency. When one provider enters "hypertension" while another types "HTN," you've just created a data silo that messes with reporting, analytics, and clinical decision support. Establishing—and enforcing—standardized data entry protocols isn't just a good idea; it's non-negotiable.
Your first move should be to prioritize structured data fields over free-text notes whenever you can. Narrative notes definitely have their place, but relying on them for core clinical data makes any kind of meaningful analysis nearly impossible.
- Lean on Drop-Down Menus: Swap out free-text fields for diagnoses, medications, and allergies with standardized, searchable lists.
- Implement Required Fields: Make sure critical information, like allergy documentation, is mandatory before an encounter can be closed.
- Create a Data Dictionary: This is your playbook. Develop a clear guide that defines each data field and its accepted values so everyone is speaking the same language.
Taking these steps cuts down on ambiguity and helps build a clean, uniform dataset you can actually rely on for everything from individual patient care to large-scale population health initiatives.
Perform Regular Data Audits
You can't fix a problem you don't know you have. That’s why regular data audits are so important for catching and correcting inconsistencies before they spiral out of control. Think of it as preventative maintenance for your most valuable asset: your data.
An audit doesn't have to be some massive, all-consuming project. It can be a focused review of a specific area, like how accurately medication reconciliation is being done or whether problem lists are up-to-date. Keep an eye out for common errors, duplicate entries, and outdated information.
Data integrity isn't a one-time project; it's an ongoing commitment. By embedding regular audits into your operational rhythm, you cultivate a culture of data stewardship where accuracy is everyone's responsibility.
These audits give you priceless insight into where your data entry protocols might be failing or where your team might need a bit more training. And of course, beyond the technical side, an optimized EHR must also follow robust data privacy principles to keep sensitive patient information safe.
Tackle the Interoperability Challenge
A patient’s health story is rarely confined to a single clinic or hospital. It's scattered across labs, pharmacies, specialists, and other facilities. Interoperability—the ability for different systems to seamlessly exchange and actually understand data—is what pulls that fragmented story together.
This is where technical standards are everything. Protocols like Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) are essentially the languages that allow all these different systems to communicate. By using APIs built on these standards, your EHR can pull in lab results, imaging reports, and medication histories from other facilities, giving clinicians a truly complete picture of their patient.
This seamless data exchange is vital for patient safety and for meeting regulatory demands. The standards governing health information are incredibly strict, as you can see from this detailed HIPAA compliance requirements checklist, making it essential knowledge for any healthcare organization.
The global push for better-connected healthcare is driving huge investments in this space. The worldwide electronic health record market is on track to hit $28.86 billion** by 2025 and is expected to blow past **$44.39 billion by 2034. This explosive growth is largely fueled by initiatives to improve IT infrastructure and interoperability, which just goes to show how central this concept is to the future of medicine. You can dive into the full research on the global EHR market growth on PrecedenceResearch.com.
Bringing AI and Automation Into Your EHR
Once your workflows are humming and your data is clean, the real game-changer is bringing intelligent automation into the mix. This is where your EHR can evolve from a documentation chore into a genuine clinical partner. Integrating AI-powered tools is the final, most impactful step in optimization, giving clinicians back their most valuable resources: time and mental focus.
This isn't just futuristic theory—these are practical tools making a difference right now. The idea is simple: let technology handle the repetitive, mundane tasks that lead to burnout and administrative overload. This frees up your team to do what they do best—practice medicine.
Let AI Handle the Note-Taking with Ambient Intelligence
One of the most exciting developments is ambient clinical intelligence. Picture this: a doctor and patient having a normal conversation, with no screen acting as a barrier. An AI tool listens in the background, transcribing the dialogue and automatically structuring it into a perfect clinical note.
This technology hits directly at the heart of the biggest complaint about EHRs—the endless hours spent typing, often long after the last patient has gone home.
- It captures the whole story: Instead of a doctor juggling typing and listening, the system gets the full, nuanced patient narrative.
- It slashes documentation time: Clinicians can walk out of an exam room and find the note already drafted, needing just a quick review and sign-off.
- It improves the patient connection: Removing the screen allows for real eye contact and rapport, which makes for a much better patient experience.
This move toward AI support is a massive trend. The EHR systems market from Coherent Market Insights shows that the industry's growth is driven by this kind of innovation. Big players like Epic Systems and Oracle Health are all-in on next-gen platforms that prioritize AI-driven insights and cloud-based flexibility for everyone from huge hospitals to small clinics.
Making Clinical Decision Support Actually Supportive
Clinical Decision Support (CDS) has been around for a while, but it’s often plagued by alert fatigue. When clinicians are constantly hit with pop-ups for minor drug interactions or routine tasks, they start to tune everything out. That’s a huge risk because a truly critical warning could easily be missed in the noise.
True EHR optimization means making CDS alerts smarter, not just more frequent.
An effective CDS alert should feel less like an interruption and more like a trusted colleague tapping you on the shoulder with a genuinely helpful piece of information.
Don't settle for one-size-fits-all rules. Work with your clinical informatics team to tailor alerts for specific roles and departments. A critical drug-allergy warning? Absolutely essential. A reminder to schedule a routine screening? That's probably better as a quiet message in a work queue, not a workflow-stopping pop-up.
Automate the Administrative Grind with RPA
Beyond the clinical side, your practice is filled with repetitive, rule-based tasks that are ripe for automation. Robotic Process Automation (RPA) uses software "bots" to handle jobs that humans typically do, like data entry, claims processing, or managing referrals.
Just think about the old-school process for a new patient referral. A staff member manually copies and pastes information from a fax into the EHR, checks insurance eligibility, and then flags it for schedulers. An RPA bot can do all of that around the clock without a single typo.
This frees your administrative team to focus on work that requires a human touch—helping a patient understand a confusing bill or coordinating complex care. By embracing smart automation, your EHR becomes more than just a digital filing cabinet; it becomes a dynamic engine for both clinical and operational success. To see how voice technology is playing a huge part in this shift, check out our guide on the evolution of medical speech recognition in healthcare.
Measuring Impact and Driving Continuous Improvement

True EHR optimization never really ends. It’s not a project you can check off a list; it’s a continuous loop of refining and adapting. After you’ve rolled out changes, the real work begins: figuring out if they actually made a difference. If you aren't measuring, you're just guessing.
This final stage is all about building a living process. You want your EHR to evolve with your organization, not become a digital relic. By systematically tracking results and listening to your users, you can make smart, data-driven decisions that deliver real value for years to come.
Define Your Key Performance Indicators
Before you can know if you've succeeded, you have to define what success looks like. Forget vague metrics like "system uptime." You need to track KPIs that get to the heart of the user experience and clinical efficiency.
Focus on numbers that tell the story of how your optimization efforts are impacting daily workflows.
- Task Completion Time: How long does it take a clinician to complete a common, repetitive task like ordering a med or charting a visit? A sharp drop here is a clear win.
- Click Reduction Rates: Literally count the clicks needed for key processes before and after your changes. Every single click you eliminate is a small victory that adds up to massive time savings and less burnout.
- User Satisfaction Scores: Don't underestimate the power of asking. Use simple, regular surveys—like a Net Promoter Score or a quick 1-5 rating—to get a pulse on how clinicians feel about the system's usability. This qualitative data is just as critical as the hard numbers.
When you can go to leadership and show a 30% reduction in clicks for a routine task, you’re not just talking about improvements—you're proving them. That kind of concrete evidence builds momentum for your next initiative.
Establish Effective Feedback Loops
Your clinicians are on the front lines, and they are your ultimate source of truth for EHR usability. Creating consistent channels for them to share what’s working—and what’s not—is absolutely essential. Don’t wait for complaints to boil over; be proactive.
Optimization is a conversation, not a mandate. The most successful initiatives are built on a foundation of trust and open communication between IT teams and the frontline staff who use the system every day.
You need a multi-pronged approach to gathering this vital feedback:
- Regular User Surveys: Move beyond the big annual survey. Send out short, targeted questionnaires after you launch a new feature or tweak a workflow. The feedback will be timely and much more relevant.
- Shadowing Sessions: There's no substitute for seeing the system in action. Have an informatics specialist or IT team member shadow a clinician for a few hours. You’ll uncover subtle frustrations and clever workarounds that you'd never hear about otherwise.
- Dedicated Feedback Channels: Make it incredibly easy for users to speak up. Set up a simple email alias or a dedicated Slack/Teams channel where they can quickly report an issue or suggest an idea without going through a clunky ticketing system.
This feedback is the lifeblood of your strategy. When a physician tells you a new template is missing a key field, and you fix it within a day, you build trust. You show them you’re listening.
Commit to Ongoing Training and Adaptation
Rolling out new features and better workflows is only half the battle. The other half is making sure people actually know how to use them. A brilliant new feature is useless if nobody knows it exists or understands why it's better.
Ditch the massive, one-and-done training events. Instead, shift your focus to providing bite-sized, just-in-time learning.
- Micro-Learning Videos: Create quick, 1-2 minute screen-capture videos that show exactly how to use a new shortcut or feature.
- "Tip of the Week" Emails: Send out a weekly email with a single, actionable tip that can help users save time right away.
- In-System Nudges: Use smart prompts inside the EHR to gently guide a user toward a more efficient way to complete a task while they're doing it.
This commitment to continuous learning is what turns good technology into great results. It’s a core principle behind many modern healthcare quality improvement initiatives, where process and technology have to work hand-in-hand. When you treat optimization as a never-ending cycle of building, measuring, and teaching, you guarantee your EHR remains a powerful asset that helps—not hinders—excellent patient care.
Common Questions About EHR Optimization
Kicking off a major electronic health record optimization project always brings up a ton of questions. I’ve seen it time and again: leaders want to know about the real costs, how much disruption to expect, and if the promised benefits will actually show up. Getting straight answers is the only way to build confidence and keep the project on track.
Let’s tackle some of the most common questions that come up when a healthcare organization decides it’s time to get more from its EHR.
How Much Does EHR Optimization Typically Cost?
This is always the first question, and the answer is never a simple number. The true cost of electronic health record optimization goes way beyond software licenses. It’s a mix of direct and indirect expenses that really depends on your organization's size, how ambitious the project is, and which EHR vendor you’re working with.
When you're building your budget, make sure you're accounting for these key areas:
- Consulting and Implementation: Most organizations bring in outside experts for this. They help with everything from workflow analysis to the nitty-gritty technical setup.
- Staff Training: This is a huge one. You have the cost of creating training materials, but the real expense is the clinical time lost when your staff are pulled away from patient care for training.
- Hardware Upgrades: You might find that your older workstations or servers just can't keep up with an updated system. Be prepared for new infrastructure investments.
- The Inevitable Productivity Dip: Let's be honest, there's almost always a temporary drop in productivity as your team gets used to new ways of working. You have to factor this in as a short-term operational cost.
Yes, the initial investment can feel steep. But the whole point is to achieve a long-term return by cutting down on administrative waste, preventing errors, and making your clinicians more efficient.
How Long Until We Actually See Results?
This is a marathon, not a sprint. You'll need some patience, but you should absolutely expect to see results in stages.
Some quick wins can pop up almost immediately. Simple things like well-designed templates or new order sets can start saving clinicians a few minutes per patient within weeks of going live. That time adds up fast and helps build momentum.
The bigger, system-wide improvements, however, take more time to surface. If you're looking for a measurable drop in medication errors or a real jump in user satisfaction scores, you're probably looking at a timeline of six months to a year.
The best approach is to set realistic expectations. Go after those quick wins to show value early on, but keep your eyes on the prize and track progress toward your larger strategic goals.
How Do We Get Clinicians On Board with the Changes?
Getting clinicians to change their habits is one of the toughest parts of any EHR project. They're incredibly busy, and a new workflow can easily feel like just another thing piled on top of an already full plate. The secret to getting them on board isn't about forcing the change—it's about genuine engagement.
You have to involve them from day one. Your physician and nurse champions need to be core members of the design team, not just a focus group you talk to once everything is built. When clinicians feel like they helped create the solution, they become its strongest supporters.
And always, always focus on the "what's in it for me." Every single change should be framed as a direct benefit to them. We’re talking less time spent on documentation, fewer clicks to place an order, or better data right when they need it. If they can clearly see how a change makes their day even a little bit easier, they'll be far more likely to embrace it.
Whisperit is the voice-first AI workspace built to unify dictation, drafting, research, and collaboration, helping teams move from intake to export in fewer steps. Discover how our AI-driven platform can streamline your documentation workflow at https://whisperit.ai.