Efficient Dictation for Doctors to Save Time & Reduce Burnout
Picture this: You see your last patient for the day, and when you walk out the door, all your charts are already done. That’s not a far-fetched dream. It's what modern dictation for doctors is making possible right now. These new AI systems can listen in on a natural conversation with a patient and turn it into a precise clinical note on the spot, transforming a mountain of admin work into a simple, background task.
The End of After-Hours Charting

For far too long, the end of a doctor's workday has meant facing a pile of incomplete charts. This "pajama time" dedicated to EHR documentation is a massive contributor to physician burnout, eating away at time that should be for family, rest, or simply being human. The old way of doing things—endless typing, clicking through clunky templates, and manual data entry—isn't just inefficient; it’s completely unsustainable.
This is where AI-powered medical dictation completely flips the script. It’s so much more than a simple speech-to-text microphone. Think of it as an intelligent assistant that actually understands the flow of a clinical conversation, picks up on complex medical terms, and formats the note correctly inside the EHR as you speak.
Reclaiming Time and Focus
The biggest promise of this technology is giving physicians back their most precious commodity: time. By handling documentation during the patient visit, it completely gets rid of the need to stay late charting. This is a game-changer. Doctors can finally be fully present with their patients, making eye contact and building real rapport instead of being tethered to a keyboard.
The immediate wins are pretty clear:
- Less Admin Work: You can literally slash hours of documentation from your daily workload.
- Better Patient Interactions: It frees you up to engage with patients on a human level, without a screen acting as a barrier.
- Higher-Quality Notes: The notes are captured in the moment, making them far more detailed and accurate than those cobbled together from memory hours later.
- Lower Burnout: By tackling one of the biggest headaches in medicine, it helps restore a healthier work-life balance.
We've come a long way. Old-school dictation meant waiting on a human transcriptionist, which was slow and expensive. Today's speech recognition technology is in a different league entirely. The global market for this software was valued at USD 1,520.3 million by 2023, and modern systems often hit over 90% accuracy on medical tasks. You can dig deeper into this market shift on grandviewresearch.com. This massive growth shows just how seriously the industry is taking these tools.
By taking over the most draining parts of documentation, AI dictation lets doctors get back to the medicine they signed up for—focusing on people, not paperwork. It's a critical first step to automate administrative tasks and put patient care back at the center of the practice.
Why Manual Charting Is Unsustainable
To really get why so many physicians are turning to advanced dictation for doctors, let’s picture a typical day dominated by manual EHR entry. It’s a relentless battle against the clock—a frustrating cycle of clicking through menus, hunting for the right templates, and endless typing. This isn't just a small annoyance; it's a massive drain on a doctor's focus and energy.
Every minute spent grappling with a clunky interface is a minute stolen from a patient. It's also another minute tacked onto an already grueling day. The numbers are staggering: for every hour of direct patient care, physicians often spend about two hours on EHR and other administrative work. This lopsided reality is a direct path to professional exhaustion.
The Hidden Costs of Clicking and Typing
The real price of manual charting goes far beyond just the extra hours. It directly impacts the quality of patient care and the well-being of the clinician. When a doctor has to split their attention between truly listening to a patient and navigating a computer screen, that vital human connection starts to fray.
This constant task-switching creates a heavy cognitive load, making it tougher to process complex information and increasing the odds of documentation errors. Over time, this treadmill of inefficiency and frustration becomes a primary driver of burnout. To dive deeper into this critical topic, you can read more about preventing burnout in healthcare and see how it links back to these administrative burdens.
The infographic below paints a stark picture of the time that simply evaporates due to these outdated methods.
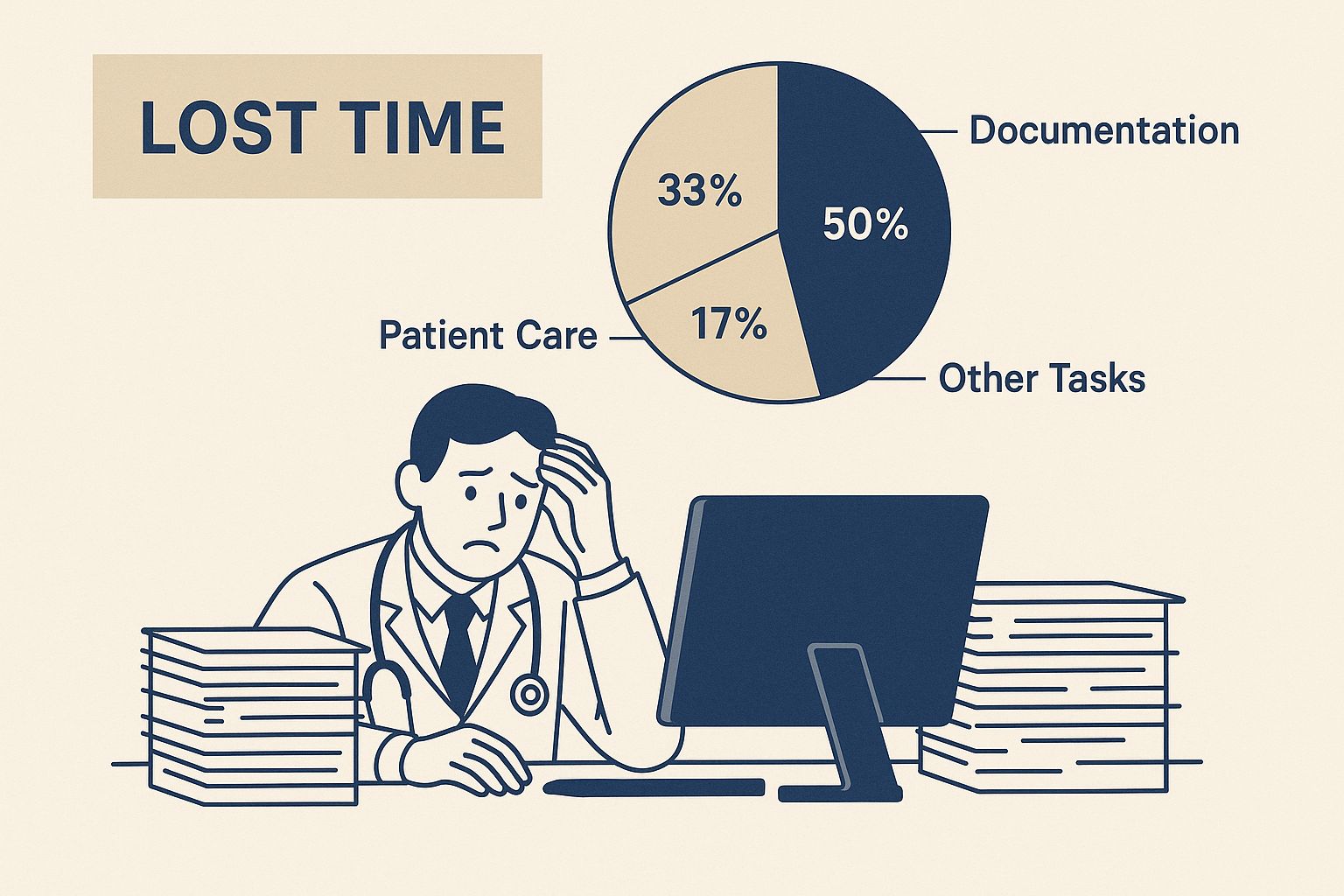
It’s a powerful visual reminder of how those "just a few minutes here and there" quickly add up, stealing precious hours from a physician's personal life every single week.
A Clear Comparison Manual vs AI Methods
When you put traditional charting methods side-by-side with modern AI dictation, the difference is night and day. One is a reactive, time-devouring chore, while the other is a fluid, real-time process that works right alongside the physician.
Let's look at a direct comparison to see exactly why manual charting is no longer a viable option for a high-performing medical practice.
Traditional Typing vs AI Dictation in Clinical Settings
The table below breaks down where the two approaches stand in terms of speed, accuracy, and overall impact on the clinical workflow.
| Metric | Traditional Typing | AI Dictation for Doctors |
|---|---|---|
| Documentation Speed | Slow and clunky, averaging 40-50 words per minute. Requires constant stops and starts. | Incredibly fast and natural, capturing speech at over 150 words per minute. Documentation happens as the visit unfolds. |
| Error Frequency | Prone to typos, copy-paste mistakes, and crucial omissions made when trying to recall details hours later. | Dramatically lower error rates, with accuracy often hitting 99% or more. Captures details in the moment, preserving accuracy. |
| Patient Engagement | Forces the doctor to split attention between the patient and the screen, constantly breaking eye contact. | Allows the doctor to maintain full focus and eye contact with the patient, building a stronger, more trusting relationship. |
| Note Completeness | Notes often end up being brief and can lack important context, as they're usually finished under intense time pressure. | Produces comprehensive, detailed notes that capture the full nuance and narrative of the patient encounter. |
| Clinician Burden | High cognitive load and a mountain of administrative work, which almost always leads to after-hours charting ("pajama time"). | Slashes the administrative workload and virtually eliminates the need to take charting home. |
This comparison really lays it all out. Sticking with manual charting means knowingly choosing a workflow that is slower, less accurate, and far more draining for physicians.
The fundamental problem with manual charting is that it forces doctors to work for their technology. A modern clinical workflow requires the exact opposite—technology that works for the doctor, fading into the background to support, not obstruct, patient care.
Making the switch isn't just about adding another piece of software. It's about fundamentally rethinking the documentation process to put the human element back at the center of medicine.
How AI Medical Scribes Actually Work
To really get what makes modern dictation for doctors so powerful, you have to stop thinking of it as just software. It’s more like having a hyper-efficient medical assistant working quietly in the background of every single patient visit. This isn't just about turning your speech into text—it’s about understanding clinical context, structuring information intelligently, and genuinely making your workflow smoother.
Let me put it this way: a basic speech-to-text app is like a court stenographer who types every single word they hear, including all the "ums," "ahs," and side chatter. An AI medical scribe, on the other hand, acts like a seasoned medical assistant who listens to the whole conversation, tunes out the noise, and then pulls out the clinically important details to build a perfect SOAP note.
This technology goes way beyond simple transcription. It’s built on sophisticated AI models trained specifically on millions of hours of real medical conversations. If you're curious about the technical journey, you can see how voice-to-text AI has evolved to handle these specialized jobs.
From Spoken Words to Structured Data
At its heart, an AI scribe is doing several key things at once while you talk with a patient. The whole point is for the system to listen passively and intelligently break down the natural dialogue, turning a simple conversation into structured clinical data without you ever having to touch a keyboard.
The real magic happens in a few lightning-fast steps:
- Real-Time Transcription: As you and your patient talk, the AI converts the audio to text with incredible accuracy. These systems have been fed massive datasets of medical terms, accents, and speaking styles, so they can nail a word like "sphenopalatine ganglioneuralgia" just as easily as "headache."
- Speaker Identification: The software is smart enough to know who's talking. It can tell the difference between your voice, the patient's, and even a family member's. This is critical for making sure the final note correctly attributes who said what—what the patient reported versus what you observed.
- Clinical Concept Extraction: This is where the AI really shows off. It doesn't just hear words; it understands meaning. It automatically identifies and tags the key clinical pieces of the encounter, like symptoms, medications and dosages, physical exam findings, and potential diagnoses.
- Note Summarization and Generation: Finally, the system pulls all this structured information together and assembles it into a coherent, organized clinical note, often right inside the EHR. It populates the right sections automatically, from the History of Present Illness (HPI) to the Assessment and Plan.
Putting It into Practice: A Real-World Scenario
Let's walk through what this looks like in practice. Imagine a cardiologist is seeing a 65-year-old patient who's been having intermittent chest pain.
Instead of typing away, the doctor just has a normal conversation. The AI scribe is listening in.
- Patient says: "The pain in my chest started about two weeks ago. It feels like a pressure, mostly when I walk up the stairs, and it goes away when I rest."
- Doctor asks: "Are you still taking the 81-milligram aspirin daily? And have you had any shortness of breath with the pain?"
- Patient replies: "Yes, I take the aspirin every morning. And I do get a little winded when the pressure is bad."
The AI processes this exchange instantly. It identifies "chest pressure" as the chief complaint, notes the onset was "two weeks ago," recognizes "exertion" as a trigger, and flags "shortness of breath" as a related symptom. It also confirms the patient is compliant with their "aspirin 81 mg" medication.
The clean layout of a typical interface allows for quick verification of the note's accuracy before it's finalized, building quality control right into the workflow.
By the time the conversation ends, a complete and accurate note is already drafted in the EHR, just waiting for a quick review and signature. This is how a 15-minute administrative chore becomes a quick, 2-minute check. To truly appreciate this leap, it helps to understand the traditional hospital scribe role and the problems it was created to solve. This technology essentially automates that entire process with far greater efficiency.
Seamless Integration with Your EHR

Bringing a powerful new tool into your practice shouldn't feel like performing major surgery on your workflow. The best dictation for doctors platforms are built to work with you, not against you. That’s why they’re designed to connect directly and securely with major Electronic Health Record (EHR) systems like Epic, Cerner, and others.
Think of it less like installing a brand-new system and more like adding a smart plugin to the software you already use every day. This integration doesn’t replace your EHR; it just makes it better. Your EHR remains the central hub for patient data, but the dictation software acts as an intelligent layer on top, making information capture faster and more intuitive.
The whole point is to get rid of the clumsy, error-prone steps that eat up your time. No more dictating into one app, then tediously copying and pasting that text into the EHR. A direct link means your transcribed note flows right into the correct patient chart and into the right fields—all in real time.
Creating a Single Source of Truth
This deep connection is absolutely critical for maintaining data integrity. When your dictation tool and EHR are perfectly in sync, you create a more reliable single source of truth for every patient's record. This has immediate, practical benefits that go far beyond just saving a few minutes.
- Eliminates Data Entry Errors: Automatic data flow gets rid of the risk of copy-paste mistakes or, even worse, putting information into the wrong patient's chart.
- Ensures Field-Level Accuracy: The best integrations can populate specific fields within an EHR template, ensuring structured data is captured correctly from the very start.
- Improves Care Continuity: With notes appearing in the EHR almost instantly, the entire care team has immediate access to the most current information, which makes a huge difference for collaboration.
This kind of smooth operation is a cornerstone of effective electronic health record optimization because it removes friction and ensures the system actually supports clinical work instead of getting in the way.
How Direct EHR Integration Works
The technology that makes this happen is designed to be completely unobtrusive. Modern AI dictation systems use secure application programming interfaces (APIs) to talk directly with the EHR. This allows the dictation software to communicate with the patient record, placing text exactly where it needs to go without any manual work.
For you, the physician, the experience is fluid and natural. You can have the EHR open on your screen, click your cursor into a field—like the History of Present Illness—and just start speaking. The transcribed text appears in that exact spot, just as if you were typing it yourself, but at the speed of speech.
This direct pathway is what completely changes the documentation game. It’s no longer a fragmented, multi-step task but a single, continuous action that can happen right during the patient encounter.
The integration of dictation systems with EHRs has already delivered some impressive results. Cloud-based solutions that let physicians dictate directly into the record have been shown to speed up documentation by 30-50% compared to typing. You can dive deeper into how these services are impacting healthcare documentation in this market research.
Ultimately, this synergy between dictation and your EHR drastically cuts down on the clicks and screen time, giving you back your focus for what truly matters: the patient sitting in front of you.
Choosing the Right AI Dictation Partner
Picking an AI partner for your dictation for doctors is a big deal. It’s not just about ticking off features on a comparison chart; it's about finding a tool that fits so naturally into your workflow you'll wonder how you ever managed without it. The wrong choice, on the other hand, can introduce a whole new layer of frustration.
Think of it like adding a new associate to your practice. You need someone who is not only intelligent but also reliable, trustworthy, and understands the unique demands of your specialty.
Not all AI scribes are built the same. Underneath the slick marketing, you'll find huge differences in accuracy, security, and the quality of support—all things that can make or break your experience. A generic, off-the-shelf dictation app just can’t handle the precision and privacy required in a clinical environment. That’s a non-starter.
To make the right call, you have to get past the sales pitch and really dig into the criteria that matter for a medical practice. This means asking some pointed questions and looking for solid proof of performance, not just promises.
Evaluating Specialty-Specific Accuracy
The first acid test is accuracy. Let's be honest, a system that constantly fumbles complex medical terms is more trouble than it's worth. General-purpose dictation tools are trained on everyday language, but medicine is its own world, with a unique vocabulary that demands specialized AI training.
When you're vetting a vendor, press them for accuracy rates specific to your field, whether that's cardiology, orthopedics, or psychiatry. A top-tier platform should have no problem showing you how well it performs with the specific terms, drug names, and abbreviations you use all day, every day.
- Ask for a live demo: Make them show you the software handling realistic, specialty-specific dictation.
- Request case studies: Look for success stories from practices that look a lot like yours.
- Inquire about the AI model: Was it actually trained on medical conversations, or is it a general model with a medical dictionary bolted on?
Taking this focused approach is the only way to ensure the tool will actually understand the nuances of your patient encounters right out of the box.
The Critical Role of HIPAA Compliance
In healthcare, data security isn’t just important—it's everything. Any dictation solution you even consider must be built from the ground up with ironclad HIPAA compliance. This isn't a "nice-to-have" feature; it's a fundamental requirement to protect your patients' privacy and shield your practice from crippling legal and financial penalties.
A truly compliant partner will be completely open about their security measures. This means end-to-end encryption for all data, whether it's being sent or just sitting on a server. They should also have crystal-clear policies about who can access data, ensuring only authorized staff can interact with sensitive information under strict confidentiality agreements.
Your potential partner must be able to provide a signed Business Associate Agreement (BAA) without any hesitation. This legal contract is your guarantee that they take protecting PHI as seriously as you do.
When a vendor puts security first, you can use their service with peace of mind, knowing your patient data is always secure. To get a better handle on the specifics, check out our in-depth guide on what it takes to be a truly HIPAA-compliant speech-to-text solution.
Integration, Support, and Transparent Pricing
Finally, let's get practical. A brilliant piece of tech is useless if it doesn't play well with your existing systems or if you can't get help when you need it.
First up, integration. Confirm that the software connects seamlessly with your specific EHR. A deep, direct integration is what you're after—something that eliminates the clumsy and time-wasting process of copying and pasting notes. The goal is simple: you speak, and the text appears automatically in the correct fields of the patient's chart.
Next, look at their implementation process and ongoing support. A good partner won’t just sell you software; they’ll have a structured onboarding plan to get you and your team up to speed quickly. They should also offer responsive, reliable tech support for any questions or hiccups down the road.
Lastly, demand straightforward pricing. Be wary of vendors with confusing fee structures, add-ons, or hidden costs. You want a simple model, whether it's a flat per-user subscription or a usage-based plan, that lets you budget accurately and clearly see the return on your investment.
The Future of Clinical Intelligence
The powerful AI-driven dictation for doctors we have today is really just the beginning. While these tools are finally freeing physicians from the keyboard, the next step is a world where clinical documentation just... happens. It fades completely into the background of the patient visit. This future is built on an idea called ambient clinical intelligence.
Imagine a system that isn't a tool you have to actively use, but more like a silent, observant partner in the exam room. That's the core of ambient technology. With the patient's permission, it simply listens to the natural conversation between a doctor and patient. No "wake words," no special commands, no pausing to dictate. It just absorbs the dialogue.
This goes way beyond simple transcription; it's about genuine comprehension. The technology is being built to understand the context of the conversation, pull out the clinically important details, and intelligently ignore the small talk.
From Transcription to True Understanding
The real leap forward is how advanced natural language processing (NLP) will soon be able to interpret and structure information, not just turn it into text. The system will recognize the chief complaint, document symptoms as they're described, and capture the review of systems and physical exam findings—all from the natural flow of a conversation.
From there, it will take the next logical steps:
- Automatically populating the EHR with structured data, putting everything in the right fields.
- Drafting a complete clinical note that's ready for the physician to quickly review and sign off on.
- Suggesting orders for labs, imaging, or prescriptions based on what was discussed.
- Identifying potential billing codes based on the complexity of the visit.
This isn't just wishful thinking; there's serious market momentum behind it. The global market for medical transcription software, which includes these AI tools, is expected to jump from USD 2.92 billion in 2025 to a staggering USD 8.41 billion by 2032. That kind of growth shows a clear and urgent demand for anything that can cut down on administrative work and fight physician burnout. You can see the full projections and get more details about this expanding market on fortunebusinessinsights.com.
A Future with Zero Administrative Burden
When you look at it this way, today's AI dictation tools are a foundational step. By mastering real-time transcription and EHR integration now, we're laying the groundwork for systems that will need almost no direct input from a doctor. The end game is to reach a state of zero administrative burden, where physicians can give 100% of their attention back to their patients.
Ambient clinical intelligence is the ultimate promise of this technology—a future where the administrative chores of medicine are automated, letting doctors practice at the absolute top of their license.
This isn't some far-off dream, either. The technology is moving fast and is already being tested in health systems. To get a sense of the broader progress, you can look at examples of Canadian Digital Health Innovation that are pushing the boundaries.
By getting on board with AI dictation now, medical practices aren't just solving today's burnout crisis—they're getting ready for a smarter, more efficient, and profoundly more human future in medicine.
Got Questions About AI Dictation? Let's Clear Them Up.
Bringing any new technology into your practice is a big deal, and when it comes to something as crucial as clinical documentation, you’re right to be cautious. For doctors and practice managers looking at AI-powered dictation, a few key questions almost always come up around security, accuracy, and how this all fits into an already busy day. Let's tackle them head-on.
The number one concern? Patient data security. Protecting Protected Health Information (PHI) is the bedrock of medical practice, so it’s a non-negotiable. The good news is that any reputable medical dictation platform is built from the ground up with security in mind. They have to be. We're talking end-to-end encryption for all data, whether it's being transmitted or just sitting on a server.
When you're vetting a service, don't just take their word for it. Insist on seeing their HIPAA compliance documentation and always get a signed Business Associate Agreement (BAA). That’s your legal assurance that they’re just as committed to protecting patient data as you are.
With these protocols in place, you can trust that sensitive information is being handled with the highest level of care.
But Will It Understand My Specialty?
This is another big one. "I'm a cardiologist. Can it really keep up with my terminology?" Or maybe you're a neurologist, and the nuances matter immensely. The answer is, yes, it absolutely can. Modern AI dictation tools often hit over 99% accuracy.
How is that even possible? These AI models aren't generic transcription bots; they’re trained on millions of hours of real clinical conversations from every imaginable specialty. The system learns your specific accent, your speaking style, and the unique vocabulary you use every day, getting smarter and more accurate with each use.
- Specialized Vocabulary: It already knows the difference between dabigatran and rivaroxaban and understands the procedures specific to your field.
- Contextual Understanding: The AI learns the context behind your notes, which dramatically cuts down on transcription errors.
- It Learns You: The more you use it, the better it gets at transcribing your dictations perfectly.
What About the Hassle of Setting It Up?
Nobody has time for a complicated, disruptive tech rollout. Thankfully, most of today's solutions are cloud-based, which makes getting started surprisingly simple. It’s typically just a lightweight software installation that plugs right into the EHR you’re already using.
Most providers will walk you through a structured onboarding process that takes less than an hour. They’ll get your voice profile set up, show you the basic commands, and get you on your way. The goal is to get you comfortable and saving time from the very first day, not weeks down the line.
And what about billing and coding? While AI dictation is focused on the clinical note, it creates a much cleaner, more detailed record. This rich documentation gives your coders exactly what they need to work accurately, which ultimately helps strengthen your revenue cycle.
Ready to eliminate after-hours charting and reclaim your time? Whisperit provides a secure, accurate, and seamless AI dictation solution designed for the demands of modern healthcare. See how it can transform your workflow at https://whisperit.ai.