Clinical Documentation Improvement Guide That Actually Works
Understanding Clinical Documentation Improvement Basics
Clinical documentation improvement (CDI) is the foundation of efficient and effective healthcare. It focuses on ensuring patient medical records accurately and completely reflect the complexities of their health status. This translates complex medical data into usable insights that improve patient care and streamline hospital operations.

Why Accurate Documentation Matters
The core principle of CDI is accuracy. This precision is critical for many reasons. First, clear, comprehensive documentation helps ensure everyone on the care team understands the patient's condition. This shared understanding reduces the risk of miscommunication and medical errors, a significant concern in healthcare.
Clinical documentation improvement is a key factor in addressing these challenges, particularly in the United States. By 2025, roughly 72% of U.S. hospitals reported patient data gaps contributing to medical errors, costing an estimated USD 17.1 billion. Learn more about these challenges: How the US Clinical Documentation Improvement Market Is Transforming.
Accurate documentation also plays a vital role in coding and billing. Proper coding ensures correct reimbursement from insurance companies and government programs like Medicare. This directly impacts the financial stability of healthcare organizations, allowing them to reinvest in resources and improve patient care. For more information on planning, consider resources like an end-of-life planning checklist.
CDI: Beyond Coding and Billing
The benefits of CDI go beyond financial considerations. Complete documentation is essential for quality reporting and measuring treatment effectiveness. This data allows providers to track patient outcomes, identify areas for improvement, and ultimately, deliver better care. It also improves communication between healthcare providers, ensuring continuity of care.
Comprehensive documentation is also crucial for research and analysis. By capturing detailed patient information, treatments, and outcomes, CDI contributes to a deeper understanding of diseases and the development of new treatments. CDI not only improves individual patient care, but also advances the entire field of medicine. For additional tips and insights, see this helpful resource: How to master clinical documentation improvement tips. This information allows medical professionals to gain critical insights into improving healthcare practices.
Why The CDI Market Is Exploding Right Now
The healthcare industry is experiencing a major shift, with clinical documentation improvement (CDI) playing a key role. CDI is no longer a behind-the-scenes function; it's now crucial for both financial stability and better patient care. But what’s driving this rapid growth? Several factors, including regulatory changes and technological advancements, are converging to create both obstacles and opportunities for healthcare providers.
The Financial Imperative: CDI and Revenue Cycle Management
One of the biggest reasons for the CDI market's expansion is its direct link to a healthcare organization's financial health. Accurate documentation is the foundation for proper reimbursement from insurers and government programs like Medicare. CDI programs ensure documentation accurately reflects the complexity of a patient's case, resulting in appropriate coding and billing. This not only maximizes revenue but also minimizes the risk of claim denials and audits.
The move towards value-based care models also highlights CDI's importance. In these models, payment is tied to patient outcomes and quality of care, both of which are closely linked to accurate and complete documentation. CDI is essential for proving the value of the care provided, which further boosts market growth. You might be interested in: How to master healthcare process improvement. The global CDI market is expected to reach USD 10.44 billion by 2034, growing from USD 5.26 billion in 2025. This represents a CAGR of 7.90%. For more statistics, visit: https://www.precedenceresearch.com/clinical-documentation-improvement-market.
Regulatory Pressures and Compliance
The healthcare regulatory landscape is constantly changing, putting more pressure on organizations to maintain precise and compliant documentation. Regulations like HIPAA and other compliance standards mandate strict documentation practices. CDI programs are key for avoiding penalties and legal problems. They also help ensure documentation meets the requirements for quality reporting initiatives, further increasing CDI's importance.
The Technology Factor: AI and Automation in CDI
Technological progress is also fueling the CDI market boom. Artificial intelligence (AI) and machine learning are changing documentation processes, making them more efficient and accurate. These technologies can spot documentation gaps, suggest correct codes, and automate tasks, allowing CDI specialists to handle complex cases. This improved efficiency and accuracy not only benefits revenue cycle management but also contributes to higher quality patient care. Improved documentation also leads to better communication, a core component of many CDI programs.
Technology That's Actually Changing CDI Today

The clinical documentation improvement landscape is constantly changing, thanks to powerful advancements in technology. These developments have a significant effect on how healthcare organizations manage and use patient data. This, of course, has major implications for both patient care and operational efficiency. Let's take a look at some of the key technologies making a real difference.
AI and Machine Learning: The CDI Power Duo
Artificial intelligence (AI) and machine learning are no longer things of the future. They're actively reshaping CDI processes today. These technologies are improving the speed and accuracy of documentation without interrupting existing clinical workflows.
AI-powered tools, for example, can pinpoint documentation gaps, recommend appropriate codes, and even automate certain tasks. This frees up CDI specialists to concentrate on more complex cases. The result? Improved efficiency and accuracy in coding and billing. For further reading on this topic, see How to master document automation software.
Furthermore, AI and machine learning algorithms can analyze large quantities of patient data to uncover hidden trends and patterns. This analytical power can result in more precise diagnoses, more effective treatment plans, and ultimately, better patient outcomes.
EHR Integration: Making the Most of Existing Systems
Effective electronic health record (EHR) integration is crucial for getting the most out of CDI technology. Some EHR integrations are truly worthwhile, while others can cause more headaches than they solve. Choosing the right EHR integration is essential for seamless data flow and efficient workflows.
The right integration can simplify the documentation process, decrease manual data entry, and facilitate communication between different departments. On the other hand, poorly implemented integrations can create data silos, disrupt workflows, and lead to frustration among clinical staff. Careful planning and consideration are vital for successful EHR integration. This progress in clinical documentation improvement is directly linked to advancements in technology and the evolving regulatory environment. In fact, the CDI market, valued at approximately USD 3.99 billion in 2024, is expected to reach USD 4.32 billion in 2025, demonstrating an 8.3% CAGR. Learn more about this in the Clinical Documentation Improvement Market Overview 2025.
Physician Buy-In: The Key to Success
Possibly the largest obstacle for many CDI technology initiatives is getting physicians on board. Clinicians can sometimes resist new documentation tools. Overcoming this resistance is paramount for the successful adoption of any new technology. Open communication, comprehensive training, and clearly demonstrating the benefits of the technology – for both physicians and patients – are all key to encouraging acceptance and ensuring long-term success. This paves the way for discussions about developing effective CDI programs.
Building CDI Programs That Actually Deliver Results
Building a successful Clinical Documentation Improvement (CDI) program isn't a matter of chance. It takes strategic planning and execution. High-performing healthcare organizations use proven frameworks to design programs that deliver measurable improvements right from the beginning. Let's explore how to build a CDI program that generates tangible results.
Strategic Planning: The Foundation for Success
Effective CDI programs start with a well-defined plan. This plan should outline the program's objectives, identify key stakeholders, and create a clear implementation roadmap. This involves evaluating current documentation practices, identifying areas for improvement, and establishing realistic, measurable goals. For example, a hospital might aim to increase documentation completeness by 10% within six months. A solid plan keeps the program focused and moving forward.
Staffing and Training: Investing in Your Team
A strong team is essential for CDI success. Different organization sizes require different staffing models. A small clinic might only need one dedicated CDI specialist, while a larger hospital system might require an entire CDI team. Comprehensive training is just as important. CDI staff needs a deep understanding of coding guidelines, medical terminology, and documentation best practices. This ensures everyone is prepared to effectively fulfill their roles.
Change Management: Turning Skeptics into Champions
Implementing a CDI program often means changing established workflows and documentation habits. This can sometimes be met with resistance, particularly from physicians. Successful change management strategies are crucial for overcoming this resistance and getting everyone on board. This involves clear communication, ongoing training, and highlighting the program's benefits for both clinicians and patients. Explaining how improved documentation leads to better patient care, for instance, can be highly motivating. Technology is transforming how CDI is implemented today. Consider this discussion of AI in Customer Success.
Implementation Approaches: Finding the Right Fit
There are many ways to implement a CDI program. Some organizations opt for a pilot program within a specific department, while others choose a full-scale rollout across the entire organization. The best approach depends on factors such as the organization’s culture, resources, and overall goals. Be sure to also consider the specific needs and challenges of your organization when selecting your implementation strategy. Workflow automation can significantly affect CDI implementation, learn more in our article about How to Master Workflow Automation in Healthcare.
The following infographic visualizes some key metrics for clinical documentation improvement, including documentation completeness rate, average query response time, and coding accuracy improvement.
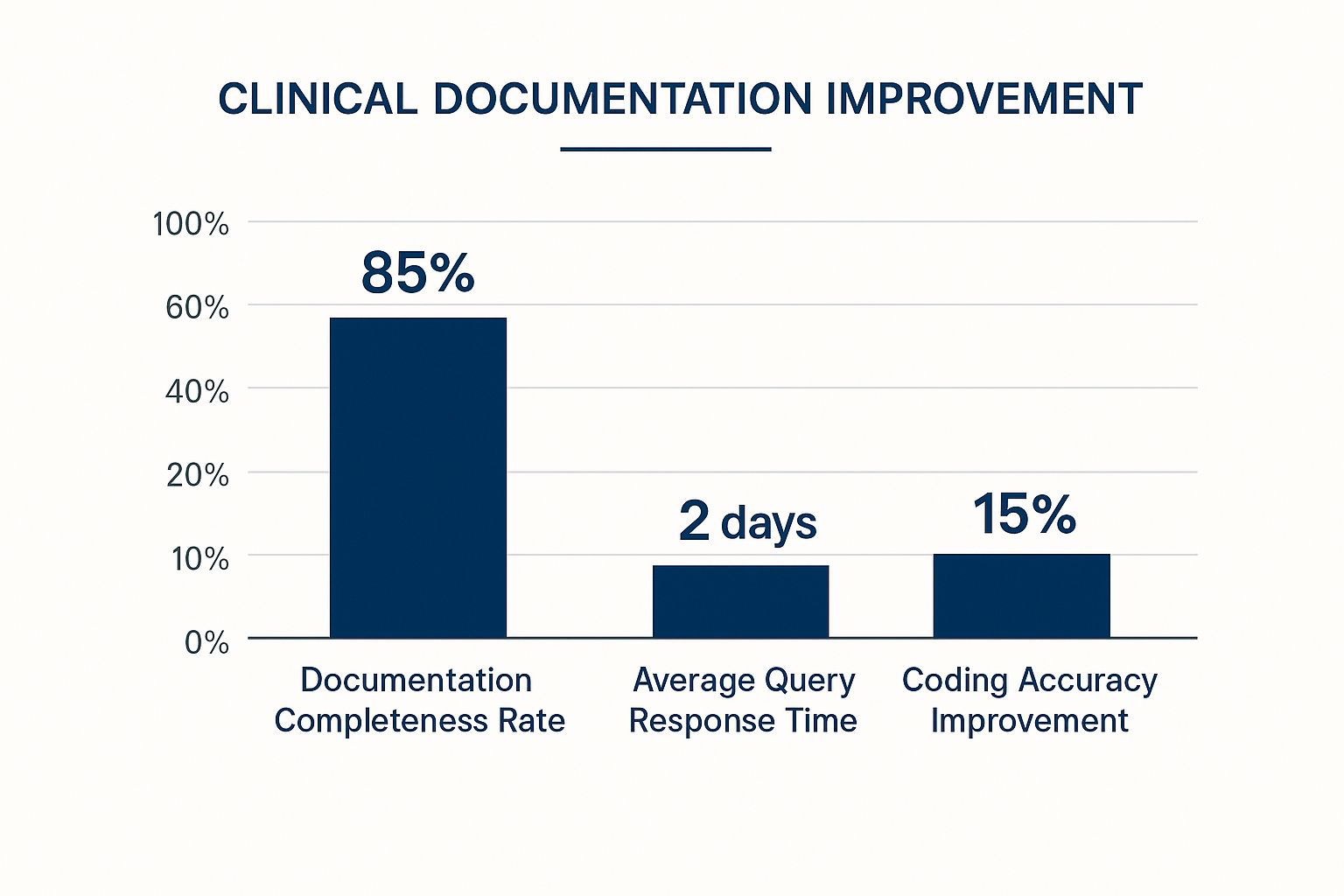
This data reveals a strong documentation completeness rate of 85%, a quick average query response time of 2 days, and a notable 15% improvement in coding accuracy. These metrics highlight the potential positive impact of a well-implemented CDI program.
To further illustrate different implementation strategies, let's take a look at a comparison of various CDI program models.
The following table, "CDI Program Implementation Comparison", details different CDI program models, implementation timelines, and expected outcomes for various healthcare organization types. It helps to illustrate how different approaches can be tailored to specific needs and resources.
| Program Model | Implementation Time | Staff Requirements | Expected ROI | Best Suited For |
|---|---|---|---|---|
| Basic Model | 6-12 months | 1-2 CDI Specialists | 2:1 - 4:1 | Small hospitals, clinics |
| Intermediate Model | 12-18 months | 3-5 CDI Specialists, Auditor | 4:1 - 6:1 | Medium-sized hospitals |
| Advanced Model | 18-24 months | 5+ CDI Specialists, Auditor, Physician Advisor | 6:1 - 8:1 | Large hospital systems, academic medical centers |
This table demonstrates how the scale and complexity of a CDI program can vary greatly based on the organization's size and resources. Smaller organizations might begin with a basic model and gradually scale up as needed. Larger organizations with more resources might implement a more comprehensive model from the start.
By addressing these elements, healthcare organizations can create robust CDI programs that genuinely achieve results. This sets the foundation for effectively measuring the program's success and continuing to optimize its performance.
Measuring CDI Success The Right Way

Measuring the effectiveness of a Clinical Documentation Improvement (CDI) program goes beyond simply meeting compliance requirements. Successful programs track indicators that matter to both clinical and financial stakeholders. This means focusing on metrics that demonstrate tangible value.
Key Performance Indicators for CDI Programs
Leading CDI programs leverage a variety of Key Performance Indicators (KPIs) to showcase their impact. These KPIs often include documentation quality scores, measuring the completeness and accuracy of patient records. The case-mix index (CMI), reflecting the complexity of patient cases, is also crucial.
Furthermore, successful programs monitor patient safety improvements linked to better documentation, such as reduced medication errors or hospital-acquired infections. These combined data points offer a holistic view of program effectiveness.
Establishing Baselines and Setting Targets
Understanding a program's true impact starts with establishing solid baselines. This involves collecting data on current performance before implementing any CDI initiatives. For instance, measuring the initial query response time creates a benchmark for future comparisons.
After establishing baselines, set realistic improvement targets. Achievable goals, such as a 25% decrease in query response time, promote progress and maintain team motivation.
Creating Actionable Reporting Systems
Effective CDI programs require reporting systems that offer insightful information, not just raw data. These systems should track relevant metrics and present them in an accessible and actionable format.
Rather than simply reporting the number of queries, the system should analyze trends and pinpoint areas for improvement. This enables CDI teams to promptly identify challenges and make informed decisions based on the data. You might be interested in: How to master reducing administrative costs in healthcare.
Communicating CDI Value to Different Audiences
Different stakeholders prioritize different metrics. Executive leadership may focus on the financial returns of the CDI program, while physicians are more interested in improved patient care. Tailoring communication to each audience ensures the message resonates and strengthens ongoing program support. This involves presenting data clearly and concisely, often using visuals like charts and graphs to highlight key findings.
Addressing Measurement Challenges
Maintaining data accuracy and managing reporting can present difficulties. CDI programs need established processes to ensure consistent and accurate data collection. This could involve regular audits or using automated data validation tools.
Additionally, simplifying reporting processes, such as automating report generation, improves efficiency and provides timely access to crucial information. This allows CDI programs to consistently demonstrate the value of accurate and comprehensive documentation.
Solving CDI Problems Before They Kill Your Program
Even the most meticulously planned clinical documentation improvement (CDI) programs can run into obstacles. Addressing these challenges proactively is essential for maintaining momentum and achieving long-term success.
Common CDI Implementation Problems
Several common problems can hinder CDI programs. A significant hurdle is physician resistance. Clinicians may be hesitant to embrace new workflows or documentation practices. Another frequent issue is technology integration. Difficulties integrating new CDI software with existing Electronic Health Record (EHR) systems can disrupt workflows and cause frustration.
Budget constraints also present a substantial challenge. Limited resources can restrict the program's scope and make it challenging to invest in necessary technology or training. Additionally, staff turnover can impede progress and create knowledge gaps within the CDI team. Finally, constantly evolving regulatory compliance requirements add another layer of complexity.
Strategies for Overcoming CDI Challenges
Fortunately, proactive solutions exist for these common CDI problems. To overcome physician resistance, focus on transparent communication and demonstrating the advantages of CDI for both clinicians and patients. For instance, clearly explain how improved documentation can contribute to better patient outcomes and minimize medical errors.
Technology integration challenges often require meticulous planning and collaboration with IT departments. Pilot testing new systems and offering comprehensive staff training can facilitate a smoother transition. Budget constraints might necessitate prioritizing crucial program components and investigating cost-effective alternatives. One approach could be leveraging existing EHR functionalities or exploring external funding opportunities to optimize resource allocation.
Addressing staff turnover necessitates investing in training and professional development to retain skilled CDI team members. Mentorship programs and opportunities for career advancement can improve morale and foster long-term commitment. To effectively manage regulatory compliance pressures, staying abreast of the latest guidelines and investing in compliance software can streamline the process and mitigate the risk of penalties.
Maintaining Momentum Despite Challenges
By anticipating and addressing these common roadblocks, CDI programs can maintain progress even when encountering difficulties. Building a successful CDI program is a continuous process requiring adaptation and constant improvement. Regular program evaluation and feedback from stakeholders can pinpoint areas for refinement and ensure lasting success. This proactive strategy enables organizations not only to solve problems but also to convert them into opportunities for growth and innovation within their clinical documentation improvement initiatives.
What's Coming Next In Clinical Documentation
The future of Clinical Documentation Improvement (CDI) is evolving, influenced by advancements in technology and changing patient expectations. This dynamic environment requires healthcare organizations to adopt a proactive and adaptable CDI strategy.
Advanced Automation Capabilities
Artificial intelligence (AI) and machine learning are playing an increasingly significant role in CDI. These technologies are automating time-consuming tasks, allowing CDI specialists to focus on complex cases and improve accuracy. Machine Learning. This shift towards automation requires CDI professionals to adapt their skills and embrace these new tools.
New Regulatory Requirements and Value-Based Care
Regulatory changes continue to shape CDI practices. Staying informed about these updates and ensuring compliance is critical for avoiding penalties and maintaining a successful program. The shift toward value-based care models further emphasizes the importance of accurate documentation. These models link reimbursement to patient outcomes and quality of care, making precise documentation crucial for demonstrating value.
Evolving Documentation Practices
Advances in voice recognition technology are streamlining the documentation process, making it faster and more convenient for clinicians. The integration of patient-generated data, such as information from wearable health trackers, provides a more comprehensive view of patient health. This integration presents both challenges and opportunities for improved care.
The Growing Importance of Interoperability
Interoperability, the ability to seamlessly share patient data between different systems and healthcare providers, is becoming increasingly important. This improved data exchange facilitates better communication and collaboration among healthcare teams, leading to more informed decisions and improved patient outcomes.
Population Health Management and Quality Reporting
The growing focus on population health management and quality reporting is also reshaping CDI priorities. Accurate and complete documentation is vital for tracking population health trends, identifying areas for improvement, and demonstrating the effectiveness of interventions.
To summarize the emerging trends and their impact, let's look at the following table:
CDI Technology Trends and Impact Timeline
Overview of emerging CDI technologies, their projected adoption timelines, and expected impact on documentation practices
| Technology | Current Status | Adoption Timeline | Expected Impact | Implementation Complexity |
|---|---|---|---|---|
| AI-powered CDI software | Early adoption | Next 2-5 years | Automated coding and query generation | Moderate to High |
| Voice recognition software | Increasing adoption | Next 1-3 years | Streamlined documentation workflow | Low to Moderate |
| Patient-generated data integration | Emerging | Next 3-5 years | More holistic patient view | Moderate |
| Interoperability solutions | Growing adoption | Next 1-3 years | Improved care coordination | Moderate |
This table highlights the projected adoption timelines and potential impact of various CDI technologies. While some, like voice recognition, are already seeing widespread use, others, such as AI-powered solutions, are still in their early stages. Understanding these trends is crucial for healthcare organizations to effectively plan their CDI strategies.
Embracing these advancements and adapting to the evolving landscape will be essential for healthcare organizations to achieve continued success in CDI.